A short protein fragment, or peptide, may lead the way to healing traumatic brain injuries, a primary cause of death and disability among youth.
Currently, drugs to treat such injuries are injected directly into the brain — an invasive technique — or into the bloodstream, which allows the medication to spread throughout the brain, causing harmful side effects. Attaching drugs to the new peptide, called CAQK, would avoid these problems. The peptide, just four amino acids long, binds to a protein complex that’s more abundant in injured areas and can therefore carry the therapy through the blood straight to the damaged sites.
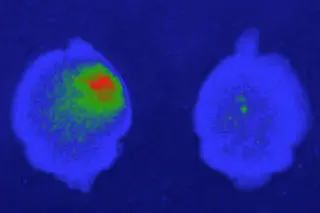
The 1-in-a-billion CAQK peptide (dark blue) also targets injured sites in human brain samples, showing its potential for precise drug delivery. (Credit: Mann et al. 2016 Nature Communications. Reprinted by permission from MacMillan Publishers Ltd)
Mann et al. 2016 Nature Communications. Reprinted by permission from MacMillan Publishers Ltd
...