Two centuries ago Edward Jenner administered the first scientifically developed vaccine, injecting fluid from a dairymaid’s skin lesion into an 8-year-old boy. The English physician knew that dairymaids who contracted cowpox, a comparatively mild skin disease, became immune to the much deadlier smallpox, which at the time killed 400,000 Europeans a year. Jenner hoped the fluid from the cowpox lesion would somehow inoculate the boy against the smallpox scourge. His hunch proved correct. Today vaccines (vaccinia is Latin for “cowpox”) of all forms save 3 million lives per year worldwide, and at a bargain price. A measles shot, for instance, costs less than a dollar per dose.
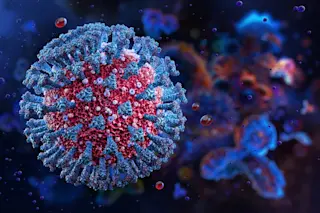
By training the human immune system to recognize and ward off dangerous pathogens, vaccines can protect against disease for decades, or even for a lifetime. Preventive vaccines work by introducing harmless microbial chemical markers, known as antigens, which resemble the markers on living ...