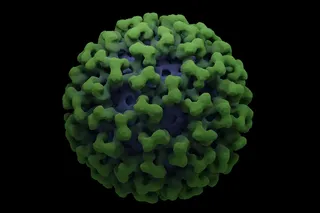
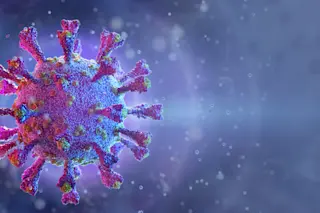
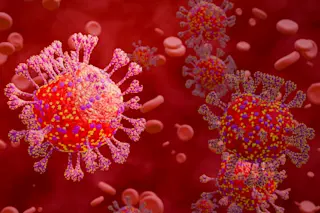
After a decade of disappointments, AIDS researchers may finally have blown the virus’s cover. A flurry of recent studies using new and more powerful antiviral drugs have captured a radically new picture of how the virus overwhelms the immune system. While it may take years for a person infected with the virus to get sick and die, that does not mean the virus is slow moving; all the while, it now seems, a silent but feverish battle is under way in the patient’s blood, with more than a billion immune cells being sacrificed each day to hold the line against a rapidly proliferating virus--which ultimately triumphs by the sheer force of its even greater numbers. This frightening-sounding picture, AIDS researchers are saying, just might--might--be good news. If the infection is caught early enough, before the tide has turned irrevocably against the immune-system defenders, combinations of antiviral drugs might hold the ...
The Race Against AIDS
Explore how new antiviral drugs for AIDS, like ABT-538, can revolutionize HIV treatment and restore immune response.
More on Discover
Stay Curious
SubscribeTo The Magazine
Save up to 40% off the cover price when you subscribe to Discover magazine.
Subscribe