Antibiotic resistance is one of the most pressing issues affecting public health today, and there is no other bacterial organism that better represents the urgency of this threat than MRSA, methicillin-resistant Staphylococcus aureus. This ubiquitous bacteria plays two roles, both as a skin-dwelling commensal and disease-causing pathogen, and is one of the most prevalent and deadly disease-causing bacteria in our communities at large and in our hospitals in particular. An early chapter of its ongoing metamorphosis from skin floral bug to virulent antibiotic-resistant pathogen took place in an unlikely setting: among a population of injection drug users living in Detroit in the early 1980s who were partaking in an unusual practice of homegrown infection prevention.
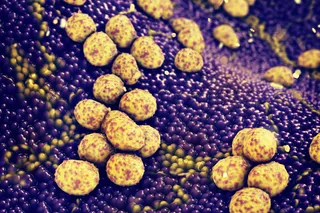
A digitally enhanced scanning electron microscopic (SEM) image of methicillin-resistant Staphylococcus aureus (MRSA) bacteria in a mustard color, which are surrounded by orange-colored cellular debris. Image: National Institute of Allergy and Infectious Diseases (NIAID). The ...