At 7 years old, Paul Michael Nelson was the kind of quiet, brilliant kid you were likely to find in Silicon Valley — captivated by Legos, self-taught in origami, loving and sweet. But on March 2, 2009, he woke up in the middle of the night, monstrously changed. He tore up the flooring in his bedroom. He got hold of a knife and stabbed holes through his door. He began speaking a strange language no one could understand. He tried pulling his teeth out. He barked like a dog.
His parents hustled their son to the psychiatrist, leading to an alphabet soup of diagnoses: ADHD (attention deficit hyperactivity disorder), OCD (obsessive-compulsive disorder), ODD (oppositional defiant disorder), bipolar disorder, autism and, ultimately, straight-up psychosis. Yet no matter what medications Paul Michael tried, treatment failed. He leaped from moving cars. He broke the windows in his room, causing the family to install Plexiglas. For the Nelsons, 2009 included 15 trips to the emergency room, two months in and out of psych wards and calls to the sheriff to remove a violent, raging Paul Michael from the home.
Finally, experts suggested that he might not suffer from a traditional psychiatric disorder caused by some inborn biochemical glitch, but from a vasculitis — a swelling of blood vessels in the brain, provoked by a hostile outside force. So the Nelsons were sent to Stanford University, where pediatric rheumatologist Jennifer Frankovich already had some experience treating the psychiatric symptoms of autoimmune disease — a frightening scenario in which the body turns on itself and attacks the brain. Twenty vials of his blood helped tell the story: Dangerously low blood platelets suggested an underlying imbalance, and signature proteins signaled some type of autoimmunity at the root.
Thus commenced years of trial-and-error therapy, conducted mostly in a psychiatric ward. Frankovich and her colleague, psychiatrist Margo Thienemann, first prescribed steroids to dial down Paul Michael’s immune response. But the symptoms abated only slightly, and his small body ballooned. Then, they shut down his immune system altogether with the chemotherapy drug Rituximab. To boost it back up and keep inflammation down, they added intravenous immunoglobulin, or IVIG, a total immune system-replacement made from the blood of thousands of healthy individuals. Frankovich hoped the approach would work, but Paul Michael’s brain was potentially damaged, she warned, and it could take years to repair. It was late in 2013 when sweet, smart Paul Michael, rescued by years of treatment, finally stepped out of the psych ward and back into his life. Today a gentle young man of 15, he goes to public school and hopes to be a pastry chef. “He’s an amazing baker,” says his mother, Mary Nelson.

For years, Paul Michael Nelson struggled with a mysterious autoimmune disorder called PANS. Thanks to pioneering research, Paul Michael, now 15, is more himself these days. Here, he cuddles with his family's kitten. (Credit: Courtesy of Mary Nelson)
Courtesy of Mary Nelson
For Frankovich, Paul Michael was patient zero — her first encounter with a newly recognized, still-controversial diagnosis called pediatric acute-onset neuropsychiatric syndrome, or PANS.
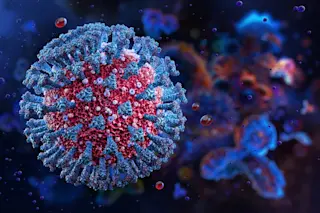
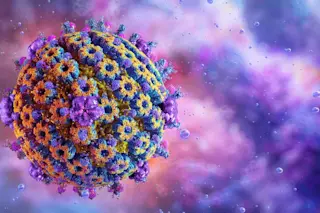
PANS is thought to be an inflammatory condition that results when an infection or some other invasive trigger spurs the body to turn on itself and attack structures in the brain. For years, scientists had focused on a single infection — group A streptococcal disease — that produced antibodies that attacked the part of the forebrain involved in forming habits, resulting in OCD. Today, the paradigm has widened into a much bigger idea that expands our understanding of psychiatric disease: A whole host of infections and other unknown triggers lead to the production of antibodies and immune cells that can cross into the brain. Depending on where these immune responses land and which brain structures they block, erode or destroy, a range of psychiatric ills can result. In one person, it could be OCD; in the next, it could be hyperactivity and inattention, anxiety, restricted eating, even hallucinations or autistic behavior.
When these symptoms are caused by immune disorders, standard psychiatric therapies that balance neurotransmitters are unlikely to work alone. Instead, immune therapies are the first line of treatment. At Stanford and elsewhere, the hunt is on for treatment cocktails that quell the inflammation and new strategies to keep a rogue immune system at bay.
Confronting a Mystery
Scientists have long known that infection can cause neuropsychiatric disease. One of the first known examples was syphilis, a sexually transmitted disease caused by the bacterium Treponema pallidum. Until we learned to treat syphilis with antibiotics, it was one of the most common causes of dementia and was frequent among the insane. Likewise, some have proposed that Bartonella, the microbial cause of common cat scratch fever, can sometimes induce anxiety, rage and psychosis. These diseases are caused by living organisms active within the brain itself. Rid the brain of the organism early enough and the symptoms subside.
But Frankovich and her Stanford colleagues were dealing with something else: damage caused by the immune response, including antibodies, the large Y-shaped proteins the body produces to fend off infections or other foreign invaders. Normally, an antibody attaches to and neutralizes the infection that provoked its formation. But in cases similar to Paul Michael’s, the antibodies also appeared to mistakenly recognize and interact with parts of the brain — a neural receptor here, a structural element there. In essence, the antibodies turned into autoantibodies: antibodies that attacked the self. They were passing from the bloodstream into the brain — something once considered rare — and attacking not just the infection, but the brain structures, too.
Frankovich and her team weren’t the first to encounter this devastating state of affairs. For decades, a respected but beleaguered group of scientists had gathered increasing evidence that one particular bacterial infection — strep — led to the body pumping out antibodies that attacked the brain, causing OCD and tics. Because they limited the syndrome to strep infection alone, they came up with the tongue-twisting label of pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections, or PANDAS.
The idea that OCD was a chemical imbalance in the brain goes back to the 1980s and psychiatrist Judith Rapoport, chief of child psychiatry at the National Institute of Mental Health (NIMH). Trying to find the right medicine for the sickest of these patients, Rapoport scanned their brains to zero in on regions involved in OCD and found increased activity in the basal ganglia, a center for movement and habits located at the base of the forebrain.
Not long after, Rapoport’s protégé, pediatrician Susan Swedo, who now leads the NIMH’s section on behavioral pediatrics, took notice. She proposed that one rare neurological disorder, Sydenham chorea, could shed some light on the OCD and tics the team had observed.
Swedo’s reasoning made sense. Sydenham is an autoimmune illness characterized by rapid, involuntary, purposeless movements, especially of the face, feet and hands. And it results as a complication of catching strep, which evades the human immune system by adapting its outer surface to resemble human biomolecules, a phenomenon called molecular mimicry. The bacteria can seem so similar to human tissue that antibodies produced against it attack human organs as well.
Left untreated for as little as five days, strep could produce autoantibodies that damage heart tissue, resulting in rheumatic fever. Sydenham chorea was like rheumatic fever of the brain, thought to occur when rheumatic fever progresses and strep antibodies (emboldened by fever) breaches the blood-brain barrier (BBB), the tight wall of endothelial cells ordinarily there to protect the brain from the outside world. Once they break into the brain, the autoantibodies attack the basal ganglia, causing the afflicted to jerk and writhe in a manner resembling the worst cases of the tic syndrome Tourette’s. Because OCD also is often accompanied by tics, though perhaps not as severe, Swedo’s medical model of Sydenham could work.
To see if the concept held — and whether Sydenham chorea even caused OCD — Swedo and her partner at NIMH, psychiatrist Henrietta Leonard, conducted a retrospective study in 1989 of three sites in the United States that had rheumatic fever outbreaks: Salt Lake City, the Ohio River Valley and Walden, Penn. Comparing children with and without Sydenham chorea, the duo found support for Swedo’s proposal: Two-thirds of children with Sydenham chorea actually had obsessive-compulsive behaviors and thoughts. A critical revelation of the study was that the OCD appeared “about two weeks to a month before the movements did, often suddenly and out of the blue,” Swedo says.
After the survey, her team at NIMH began seeing Sydenham children who were at the height of the disease. “We brought them in from all over the United States, and you couldn’t make these stories up,” Swedo says. “One of the boys had a very classic fear that school was contaminated and made his brother leave his shoes outside the house. Then they stepped inside the house and they had to take their socks off. And his mother had to wash those socks right away.”
As a pediatrician, Swedo felt compelled to help these children with Sydenham, but neuropsychiatric medications focused on rebalancing brain chemistry just didn’t work. So she began to consider treating the autoantibodies themselves. By the early 1990s, Swedo and the NIMH team were treating the Sydenham group and pioneering some of the same types of treatments used for patients like Paul Michael today: steroids such as prednisone to stanch the tide of immune molecules; plasmapheresis, a technique to filter the blood, cleanse it of autoantibodies, and return it intact to the patient; and intravenous delivery of a new, healthy immune system with IVIG.
But as Swedo and colleagues studied data from the drug trials for their Sydenham patients and controls without the disease, they found something else. Not just in the extreme situation of Sydenham’s, but even with ordinary strep, autoantibodies appeared to careen though the brain, causing less severe forms of tics and OCD.
Discovering a New Disease
Ultimately, three brothers in Swedo’s clinic helped her grasp what was going on: The oldest had a diagnosis of Tourette’s syndrome with physical tics. The second child had some tics. And the youngest had tics and movements so extreme that doctors diagnosed him with Sydenham chorea.
“He also presented to the clinic with very severe hoarding,” Swedo recalls of the youngest. “He carried a brown paper bag with him and if he saw a piece of paper, he’d put it in the bag. After he came the first time, we had enough sense to clear the magazines out of the waiting room.” The child also had an “incredibly complex tic where he waved his arm around just huge and he also was kind of floppy.”
But the youngest brother, it turned out, did not have Sydenham. Instead, he had developed his psychiatric symptoms as the result of a more ordinary strep infection. “He was the first PANDAS case,” Swedo says. The boys’ mother, a medical technologist, helped to connect the dots. Her eldest son, the one diagnosed with Tourette’s, had tics that waxed and waned. Whenever his symptoms reached a peak, his throat cultures tested positive for strep. Now Swedo and her team saw the picture clearly: Ordinary strep infection could cause neuropsychiatric symptoms in a far broader, more under-the-radar group of patients.
The strep model worked perfectly for Tanya Murphy, a University of South Florida psychiatrist who’d been observing the infection’s footprint for years. Murphy had found that right after strep, psychiatric ills could suddenly manifest: not just OCD, but eating disorders like anorexia. “And these weren’t typical anorexia patients worried about body image,” she says. Like the OCD patients themselves, “mostly, they were worried about contamination.”
Murphy’s work, which spans two decades, helped to define the population in a nuanced way. As early as 2006, she established that children with OCD from PANDAS had truly toxic behavioral reactions to the same dose of serotonin-based medications that brought relief to those with standard forms of OCD. It was clear the two groups were not the same.
One of her most important contributions, published with Swedo in Biological Psychiatry in 2007, was based on a study of about 700 children, ages 3 to 12, all healthy at the start. Murphy followed the children for eight months, continually swabbing and testing for a strep infection, looking for signs of OCD and tics. By the end of the study, she had found a clear association between strep and the neuropsychiatric symptoms.
That connection was strengthened by immunologist Madeleine Cunningham, a rheumatic fever expert from the University of Oklahoma. Swedo recruited her in 1999 to explore what autoantibodies from strep could do to the brain. It was a wild ride. Cunningham and her postdoc at the time, Christine Kirvan, found that the antibodies literally bind to human neurons, activating an enzyme called calcium/calmodulin-dependent protein (CaM) kinase II. When patients had high levels of activated CaM kinase II floating around in their brains, nerve cells got overstimulated, and symptoms of OCD or a movement disorder could erupt. The protein marker offered a blood test for PANDAS.
But that represented just part of the damage. Cunningham found that the same patients produced autoantibodies targeting lysogangliosides, molecules within the membranes of nerve cells in the brain. Although it hasn’t been demonstrated yet, autoantibodies attacking these lysogangliosides are thought to disrupt nerve cell signal transmission and, presumably, the behavior of the patients. The autoantibodies also attached to tubulin, a protein molecule used to maintain a cell’s physical structure. Cunningham suspects that when the strep antibodies target tubulin in the brain, the result is a gumming up of a cell’s structural machinery and, apparently, neuropsychiatric ills. More recently, Cunningham has found that strep antibodies target brain receptors for dopamine, a neurotransmitter important for cognitive focus.
Settling a Dispute
For years, such findings were met with the salvos of critics insisting the very notion of PANDAS was a fantasy — an absurd concept at loggerheads with neurology and logic.
How ridiculous, those critics said: Since 60 to 70 percent of children catch a strep infection at some point, naturally those with OCD or tics would, like everyone else, show evidence of exposure in their blood. Swedo, Murphy and others claimed that tics in kids with PANDAS appeared suddenly, yet, critics argued, the same was true for tics in Tourette’s, so how could you tell them apart?
“Until more definitive scientific proof is forthcoming,” neurologist Roger Kurlan and pediatrician Edward Kaplan wrote in Pediatrics in 2004, there was “insufficient evidence” to justify strep testing in children with neuropsychiatric symptoms. And most assuredly, there was not enough proof to treat these patients with antibiotics or immune-modifying therapies and drugs.
The dispute came to a head in 2010 at a contentious meeting at the National Institutes of Health. Swedo, Cunningham, Murphy and crew dropped their claim that the phenomenon caused tics (“even though we usually see them,” Swedo says). But they and critics in the field were able to agree that infection wasn’t a necessary trigger for symptoms, widening the scope of the phenomenon way beyond strep.
The field has moved on, emerging from the meeting with a new name for the devastating illness: pediatric acute-onset neuropsychiatric syndrome, or PANS. Writing in Pediatrics and Therapeutics in 2012, Swedo, along with Jim Leckman of the Child Study Center at Yale University and the famed Johns Hopkins University immunologist Noel Rose, set the criteria for PANS. To meet the diagnostic bar, patients would have to manifest abrupt, dramatic onset or recurrence of either OCD or an eating disorder like anorexia. They would also need to have at least two of seven additional symptoms: anxiety; sensory or motor abnormalities; developmental regression; irritability and aggression; deterioration in school performance; mood swings or depression; and things like frequent urination and insomnia. Doctors also had to first rule out other disorders, like lupus or Tourette’s.
A New Diagnosis of Hope
Now, researchers have further refined their understanding of the syndrome, and a series of powerful new studies published over the past couple of years have helped establish autoimmunity’s role in neuropsychiatric disease.
In the time since that tense 2010 NIH meeting, Murphy set out to study 43 children recruited soon after the sudden onset of OCD, capturing the early characteristics of the disease. The children were so impaired that a third of them had to be home-schooled. A large number had trouble eating due to fear of food; one was so dehydrated she was sent to the ER. Infectious triggers included strep and the bacterium mycoplasma.
Given these findings, Murphy treated the kids with azithromycin, an antibiotic that targets both infections. And she saw improvement, especially in kids with the most severe tics.
In 2012, Jennifer Frankovich opened the doors of her multidisciplinary PANS clinic, and patients flooded in. Whereas Murphy’s patients were selected for the recent onset of symptoms, the children arriving at Stanford had progressed to advanced stages of the disease without appropriate treatment. And so, like Paul Michael Nelson, they seemed intractably ill. “Many kids were disabled by their psychiatric symptoms,” Frankovich says. “They had OCD with severe intrusive thoughts, deep anxieties and fears, panic, rage.” They also had cognitive problems: handwriting deterioration, slow processing speed and regressions so frightening that a once-normal 10-year-old might have the skills and behavior of a developmentally slow 3-year-old.
Tracing each illness back to the start of symptoms, Frankovich has managed to find clusters: groups of children from the same school or neighborhood who had all come down with the condition in the same month; individuals with a true, physical connection, like the family of three brothers Swedo had studied years before. In the course of her investigation, a host of alternate infections have emerged: not just strep, but bacterial mycoplasma, influenza, sinusitis, pneumonia and others.
By 2015, Frankovich and her team had led the effort to create treatment guidelines for PANS patients. Though many young people in the Stanford PANS clinic had OCD, their psychiatric illnesses went well beyond that: 40 percent had suicidal thoughts; 19 percent had homicidal thoughts; and nearly two-thirds were at risk of committing violent acts. Some 26 percent had psychosis. This wide assortment of symptoms has Frankovich on a quest to identify subgroups in the hopes of tailoring treatments, but she longs for the day she can find and use a full array of biomarkers signaling disease and genetic risk. “Maybe we really have 10 disorders,” she says. “Maybe strep-triggered PANS is different from flu-triggered PANS. This is a real disease, but we need more research to learn where the true lines lie and many treatment trials to understand the best therapies.”
Peering Into the Brain
One promising tool is the “Cunningham Panel,” created by Cunningham through her commercial lab, Moleculera. Currently used for patients with neuropsychiatric symptoms, blood tests in the panel search for the autoantibodies Cunningham has found. The tests also look for whether the blood increases CaM kinase II activity.
The panel is so nuanced that it measures the level of autoantibodies against two types of dopamine receptors. Cunningham has come up with a formula based on the ratio of autoantibodies to the two dopamine receptors; depending on the balance between the two, she can predict a variety of symptoms, from ADD to compulsions to obsession to irritability and more. If a patient’s blood shows high levels of the markers, it indicates that neuropsychiatric symptoms could stem from autoantibodies created in the wake of infectious disease — and that the treatment of choice might be steroids or IVIG.
The real hope, of course, is for more effective treatments targeting the underlying problem to replace these harsh therapies. Toward that end, potentially game-changing research comes from Dritan Agalliu, a vascular biologist and blood-brain barrier expert at Columbia University Medical Center in New York. Funded to focus on PANS by two wealthy parents whose child was diagnosed with the disease, Agalliu began searching in 2012 for controls to the trap door that autoantibodies use to sneak into the brain.
He exposed specially bred mice to strep and scrutinized their brains after death. How did repeated strep infection alter the integrity of the BBB? How did it induce rapid onset of neuropsychiatric disease?
One finding was that strep eventually led to massive production of a certain kind of immune cell, Th17, along with inflammation of the brain. In humans and rodents alike, Th17 cells take on the role of a conductor, telling other immune cells what to do. They have been implicated in the destruction of the BBB and are found in increased numbers in many autoimmune diseases. In the experimental mice, Agalliu saw that Th17 cells had poked holes in the BBB, opening the floodgates into the brain. Inside the brain, strep bacteria were nowhere to be found, but there were plenty of antibodies normally kept out by a healthy BBB.
Agalliu also found that Th17 cells induced by strep opened the BBB only in certain spots: Since strep enters the body through the nose, it made sense that he saw the BBB was pierced near the olfactory bulb, the structure in the front of the brain that processes odors. But strep also caused a leak in the BBB near the amygdala, the seat of fear and anxiety, and the lateral hypothalamus, where our sense of hunger begins. Given the primary PANS symptoms of OCD, anxiety and anorexia, this fit quite well. It’s possible that finding ways to repair the BBB or safely block Th17 cells would better treat PANS patients.
Another potential tactic involves pumping the immune cells and toxic molecules out of the brain — considered a futile quest until just a couple of years ago. That’s when University of Virginia neuroscientist Jonathan Kipnis and his team discovered a hidden core of vessels — a previously unknown sewage system for draining cellular waste from the brain into the lymph system at large. The work is in mice, but preliminary evidence suggests humans have it, too.
“Its existence,” Kipnis says, “could explain how Alzheimer’s plaque can be cleaned out by some of us but left for sludge in those who get disease. In some people, the vessels no longer work efficiently.” The point for PANS: In diseases of autoimmunity, where rogue immune cells are stuck in the brain, returning these lymphatic vessels to greater function may be a potent means of clearing up disease.
These newest discoveries are so early that they won’t enter the therapeutic arsenal without a wealth of additional research. And even where therapies have a track record, physicians (and parents) must differentiate between psychiatric disease, infectious disease and autoimmunity with care. Perhaps the best guideline here is that when psychiatrists call patients untreatable and show them the door, it only makes sense to explore PANS as another possible cause.
That unlikely detour brought reprieve to Paul Michael Nelson and his parents, who spent four years navigating violent rages and psychotic symptoms so overwhelming that the boy seemed forever lost. The Nelsons feared their child was, in many ways, dead. Tamping down his overactive immune system brought him back.
A Syndrome Evolves
PANS is just the latest acronym for the constantly evolving neuropsychiatric disorder. Here's the name game researchers have played to get there and how those names fit into our current understanding of the syndrome:
In 1995, in the Journal of the American Academy of Child and Adolescent Psychiatry, Susan Swedo and Henrietta Leonard reported on five cases of a syndrome they called PITANDs — pediatric infection-triggered autoimmune neuropsychiatric disorders. Their sweeping hypothesis held that OCD and tics could be triggered or exacerbated by a host of infections, including strep, influenza and chickenpox.
In 1998, Swedo pulled back from this broad-brush theory, focusing just on strep to raise awareness and create a medical model to speed discoveries. She renamed the syndrome PANDAS, for pediatric autoimmune neuropsychiatric disorders associated with streptococcal infection.
In 2010, Swedo and her colleagues met at NIH, and in a wide-ranging, collaborative group decision, they eliminated the requirement for any specific infection as a bar for the syndrome. The name of the syndrome, published officially in a 2012 paper, is now PANS, for pediatric acute-onset neuropsychiatric syndrome.