Clodomiro Picado, one of Costa Rica’s foremost scientists, conducted research on venomous snakes in Central America in the early-20th century and advocated for better products tailored to the types of snakes that lived in the area.
The institute now named after him — the University of Costa Rica’s Clodomiro Picado Institute — is one of few in the world helping people bitten by snakes in Latin America and Africa. Before the institute was created, people in Costa Rica and surrounding countries often relied on antivenoms from as far away as Brazil or elsewhere.
The trouble is, antivenoms must be tailored to a particular species.
This is partly due to venoms naturally being tailored to the prey that lives in a particular area. In some cases, even the venoms of snakes within the same species differ substantially; antivenom based on the deadly fer-de-lance from Brazil, for example, may not be as effective in Central America.
Therefore, the first step in making the right antivenom is finding the right kind of snake.
Read More: 10 of the World’s Deadliest Snakes
How Is Antivenom Made?
The Clodomiro Picado Institute currently houses more than 100 snakes. These include fer-de-lances — responsible for about half of the venomous snake bites in Costa Rica — and a large number of coral snakes.
The researchers extract venom from these serpents, then inject small amounts into horses kept in pastures on their large property. Once the horses have had enough time to produce antibodies in response to the venom, the scientists extract their blood — antibodies and all — and purify it.
The horse has been the industry’s go-to donor animal for more than a century. Why? Well, the large and docile creatures carry a lot of blood.
To make sure the horses don’t become too drained, the researchers also re-inject blood into the animals to compensate for what they lose, says Andrés Hernández Bolaños, chief pharmacist at the Clodomiro Picado Institute.
This is how to make antivenom in the most basic sense. But in practice, the researchers must ensure their products are as widely applicable as possible. After all, in the dark or in the middle of the bush, victims won’t always know what bit them.
Because fer-de-lance snakes have slightly different venom in different areas, for instance, the researchers mix in venom taken from snakes on the Atlantic and Pacific coasts of the country before injecting it in the horses.
The product that comes out of this process, PoliVal-ICP, can treat bites from the fer-de-lance and “most of the vipers of medical importance in Central and South America” — including the bushmaster and Central American rattlesnakes, as well as nearly 40 other venoms.
Read More: Deadly Animal Venom Could Lead To Pharmaceutical Breakthroughs
Testing How Antivenom Works
The institute, of course, has done a whole lot of research into how much, how often and what mixture of venoms they must inject into horses to extract the most effective serums. They’re even developing a product for scorpion venom.
But antivenom isn’t easy to test.
It’s not like researchers can just throw people into snake pits and then give them medicines to see what works. They also can’t give placebos to real-life snake bite victims, in order to compare them with non-placebo doses.
Developing a clinical study is difficult, too, given the circumstances of those bitten. While Costa Rica has about 600 fer-de-lance viper bites every year, for example, only about three to five bites come from coral snakes. Additionally, many victims are bitten in remote areas.
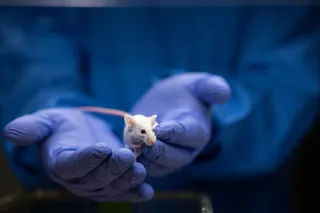
At the Clodomiro Picado Institute, the researchers instead use mice — first injecting the rodents with snake venom, then giving them antivenom to see what works. When half of the mice survive, the researchers tinker with the numbers, calculating what would work with humans.
The antivenom itself is delivered intravenously, in an IV drip. First, a doctor must try to determine which species bit the victim and whether venom was injected at all (snakes sometimes do what’s called a “dry bite” instead).
Then, a small amount of the correct antivenom is introduced to make sure there is no adverse reaction. Some people’s blood will reject the horse blood, producing allergy-like symptoms or worse. Roughly 20 to 25 percent of all people experience adverse reactions to antivenoms.
But after 15 minutes, if no reaction is detected, more antivenom can be administered. Patients are observed until their blood coagulation becomes normal and, by observing how effective mixtures are over time, researchers can hone the mixtures of their antivenom products.
The Issue With Making Snake Antivenom
The ongoing problems with making antivenom have to do with funding in most cases. There are several different species of coral snakes with dangerous bites, for example, but the low number of victims per year dissuades private drug companies from making an antivenom.
There just isn’t much profit behind it.
“Making antivenoms is not going to get you out of your house and into a mansion,” Hernández Bolaños says. “It’s actually something that the private sector is getting away from.”
Meanwhile, public health institutes in more developed countries, with better capacity to make antivenom, don’t have as much of a venomous snake problem compared to developing countries in Latin America or Africa.
For these reasons, some major antivenom manufacturers have stopped making the stuff. It’s why the Clodomiro Picado Institute, a public institution, now makes a product for the venomous snake bites commonly experienced in parts of Africa — like those from carpet vipers, puff adders and spitting cobras.
But the problem of access remains, well, a problem.
Many people are bitten hours or even days away from the nearest hospital or clinic that carries antivenom. By the time they do arrive, antivenom products aren’t effective enough to save limbs or, in the worst-case scenario, lives.
Read More: What To Do (and Not Do) If A Snake Bites You