Touring a building with Jessica Green can be an unsettling experience. “We live nearly 90 percent of our lives indoors, but we know almost nothing about that environment,” she says as we push through the doors of the Lillis Complex, a four-story glass and concrete building on the University of Oregon campus in Eugene. “We don’t think about the wildlife in the air because we can’t see it. But it’s here.”
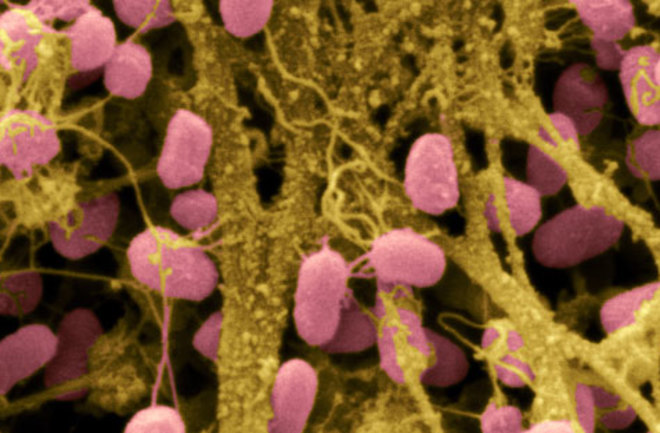
Inside the atrium, dozens of students bustle past on their way to class. Others chat with friends, send text messages, and order coffee from a small café. Meanwhile, in the air flowing around us and into our eyes, noses, mouths, and lungs, millions of microbes fight for survival. “Air isn’t empty,” Green continues. Not even close: A cubic meter of indoor air contains up to 10 million cells of bacteria. “Each one of us is shedding microbes from our bodies and resuspending microbes that have settled on the floor, on desks, on trash cans. They’re swirling all around us. We’re constantly walking through a microbial soup.”
Few scientists know more about that soup than Green, a 42-year-old theoretical ecologist and the director of the University of Oregon’s Biology and the Built Environment (BioBE) Center. Created just two years ago, the BioBE Center has quickly become a global hub for research into the biology of the great indoors. At the center, microbiologists collaborate with architects and evolutionary ecologists on research that may ultimately influence how buildings are designed and constructed in the coming decades. They believe creating a healthy indoor microbial environment is not merely a matter of wiping desks and mopping floors. Green says it has to start at the beginning, with the earliest conception in the architect’s mind.
To Green and her BioBE collaborators, the Lillis Complex is one giant petri dish. They have spent months sampling the microbes living in the building’s air and on floors, desks, chairs, and other active surfaces. The resulting DNA dataset will help them understand how the building’s various microbial populations function and interact. “Since Lillis was so recently built, we have a really good picture of the airflow through it,” Green says. “There are 12 HVAC units”—heating, ventilation, and air-conditioning—“that draw outside air in and route it through nearly 300 rooms. From each room a stream of air moves into the hallway, and they gather like tributaries into the river of this atrium, which draws warm air up and out vents in the fourth-floor atrium ceiling.”
As Green speaks, I start to feel like Keanu Reeves after he swallows the red pill in The Matrix. Just as the world around Reeves revealed itself as nothing but binary code, so the air around Jessica Green clouds up with imagined microbes. They’re kicking up in Pigpen-ish plumes at our feet. I mention this to her and she smiles. “In a way, it is kind of like that,” she says. “We walk into a room and create a microbial dust storm.”
Energized by new DNA-analysis tools and an infusion of grant money, indoor ecology has rapidly transformed from a neglected field into one of biology’s hottest specialties. In the past few years a number of leading outdoor microbiologists have come inside. Green spent her early career researching microbes on lonely field expeditions to the Arctic. Norman Pace, a University of Colorado biologist famous for his discoveries of new microbial species in the hot springs of Yellowstone, has set up one of the nation’s most productive indoor microbiology labs. North Carolina State University biologist Rob Dunn now studies household microbes.
Brendan Bohannan, director of the University of Oregon’s Institute of Ecology and Evolution, is one of the world’s experts in the microbes of the Amazon rainforest, but he’s gone indoors, too, working alongside Green at the BioBE Center. “All the beauty one would experience outdoors is in here as well,” Bohannan tells me in his BioBE office. He raises his arms to the walls. “All this diversity of life is flying around the room.”
Next Page: A DNA Revolution Heads Indoors
Their research is already yielding surprising results. Pace’s studies of residential showers have raised serious concerns that showerheads may act as delivery vehicles for bacteria that cause pulmonary disease. Dunn’s microbial transects of the American house are turning up shocking similarities between the ecosystem of your pillow and that of your toilet (see “Mapping the Home’s Microbe Habitats,” page 5). And you don’t even want to know what is turning up in detailed analyses of public bathrooms.
It’s enough to make anyone into a hypochondriac. But to Green and her colleagues, all of these studies are just fodder for a larger discussion about the ecosystem of the indoors.
For more than a century, humans have attempted to wipe out microbes with disinfectants, antibacterial solutions, and antibiotic drugs. Based on the latest discoveries, Green and her colleagues are questioning that strategy. Maybe the path to indoor health is not a ‘Kill ’em all’ approach but one of encouraging a diverse ecosystem in which benign and beneficial microbes crowd out the pathogens. “Indoor homogeneity is something we as a culture have become accustomed to,” Green tells me as we exit the Lillis Complex and breathe in the fresh Oregon air. “We’ve come to expect every room to be the same temperature, the same humidity, have the same flow of air. But rarely in the outdoor environment has homogeneity been good for an ecosystem.”
The natural world functions best with a rich diversity of species, both at human scale and in the microbial universe. Yet we spend huge amounts of money, time, and effort trying to wipe out the diversity of microbial species indoors.
Microbial dynamics are especially critical in hospitals, where bacteria like Staphylococcus aureus can weaken and kill patients who have compromised immune systems. “Hospital-acquired infections kill 2,000 people every week in this country,” Green says. “That’s nearly three times the number of people who die in highway car accidents per week.” Paradoxically, finding ways to encourage more microbial ecosystems in hospitals might help bring the number of infections down and is one of the BioBE team’s primary challenges.
In hospitals, at work, at home, we are constantly surrounded by invisible life. “It’s there whether we like it or not,” says Rob Dunn. “The only choice is which invisible life we will be surrounded by.”
A DNA Revolution Heads Indoors
Scientists began thinking about indoor environments in a systematic, ecological way in part because of the fall 2001 anthrax attacks [pdf]. Over the course of 22 days, powderized anthrax—a potentially deadly bacterium—was mailed to U.S. Senate offices in Washington, D.C., and to media outlets in New York and Florida. Seventeen people were sickened and five died after inhaling the anthrax spores.
Chemist Paula Olsiewski directed the Alfred P. Sloan Foundation’s funding initiative on biosecurity from 2000 to 2010. When she first began studying how HVAC systems could take anthrax out of the air, she made inquiries about the state of the science of indoor biology. Olsiewski found that the field was practically nonexistent, so she asked Norman Pace and J. Craig Venter, the pioneering geneticist, to look into the possibilities. As it happened, her request coincided with the introduction of a new generation of DNA tools that were about to revolutionize the entire field of microbiology.
For nearly 100 years, the only microbes that biologists could study in detail were those that could be cultured—grown in a petri dish. Unfortunately, as few as 1 percent of all microbes respond to culturing. The rest were essentially invisible to science. That situation changed only with the development of high-throughput DNA analysis. “About 10 years ago you could characterize a few hundred species through RNA sequencing,” says Jonathan Eisen, a microbiologist at the University of California, Davis. “Each RNA sequence would cost up to $100. Then about five years ago, next-generation sequencing methods became available. That made sequencing easier and orders-of-magnitude cheaper.” Nowadays, Eisen says, his lab can generate a billion RNA sequences for about $10,000. Earlier this year at the American Association for the Advancement of Science annual meeting in Vancouver, he proposed the creation of a DNA-based “field guide” to microbes from all over the planet—something that would have been prohibitively expensive just a few years ago. “High-throughput analysis flipped the cost, from hundreds of dollars per sequence to hundreds of sequences per dollar,” he says.
Armed with the new technology, Norman Pace began a series of indoor microbial explorations. He had long been fascinated by waterborne microbes, so he set his sights on the organisms that make their homes in the shower. Between 2006 and 2008 his team took apart 45 showerheads from homes, apartments, and public buildings in Denver and other cities in Colorado. They swabbed shower curtains and the showerheads, then analyzed the DNA. The results blew his mind: “Once I recognized what was going on, I said, Jesus Christ, what kinds of organisms am I inhaling?”
Pace found both the curtains and the showerheads teeming with bacterial life. “That soap scum on the shower curtain isn’t soap scum,” he says. “It’s a microbial biofilm. And it’s also living in the showerhead.” Most of the life in those biofilms was benign, made up of the kinds of microbes commonly associated with soil or water. But a distressing number of showerheads contained significant loads of Mycobacteriumavium, a bacterium that can cause nontuberculous mycobacteria disease, or NTM, a pulmonary infection that can feel like an unshakable flu. “That steam you’re breathing in the shower isn’t just steam,” Pace says. “It’s full of aerosolized bacteria, and you’re sucking it deep into your airways.”
Inspired by Pace’s findings, the Sloan Foundation’s Paula Olsiewski put out a call for proposals for a full-scale indoor environments project. She was ready to put the foundation’s financial muscle behind the nascent field. But she did not want the funding limited to microbiologists; Olsiewski wanted architects in on the research too. “If biologists are just sampling the buildings, they’re missing the point,” she says. “We want to know what’s in a building, but we also want to know what those microbes do, how they evolve and react to changes in the built environment.”
Hospitals were at the top of Olsiewski’s list of research targets. “Most people are now aware of hospital infections and how they can kill us,” she says. “Whatever strategies hospitals have been using to address the problem have not been working.” The Centers for Disease Control and Prevention (CDC) reports that 1.7 million patients pick up harmful microbes—most commonly staph infections, named for the Staphylococcus aureus bacterium—in American hospitals every year. And while millions of dollars go into hospital-associated pathogen research every year, until now no one had studied the hospital as an ecosystem, looking at the biodiversity of the total microbial population instead of just pathogens in isolation.
Jessica Green was eager to take on the challenge. A rising star in the microbiology world, Green is known as an adventurous scientist and a fearless athlete. In her younger days she competed in Roller Derby under the nom de guerre Thumper Biscuit. She had spent her career collecting microbes in the wild, but the notion of switching her focus to indoor microbes appealed to her. “I’ve always been interested in the forces that organize ecological systems, what affects the distribution and abundance of species,” she says. “This was a way to ask those questions in an almost completely uncharted environment.”
Across campus, Green had a secret weapon: G. Z. “Charlie” Brown. A leading expert on sustainable buildings, Brown directs the University of Oregon’s Energy Studies in Buildings Laboratory, where researchers test ways to make structures, including hospitals, radically more energy efficient. “Buildings account for 40 percent of energy use in the developed world,” Brown says. “Hospitals are a big part of that. They require an enormous amount of energy. A little improvement in their energy use can make a big difference.”
Ventilation systems in particular are notorious energy hogs. “Hospitals often try to solve problems of indoor air quality and infection transmission with high ventilation rates,” Brown says. In other words: Crank up the fans, flush the bad bacteria. If architects knew more about the bacteria in hospitals, Brown thought, they could design less energy-intensive ways of keeping the air clean. But the available data were sparse. “We’ve got a lot of material on airflow,” he says, “but very little on microorganisms.”
Brown had already collaborated with some of the nation’s major hospital designers, like ZGF Portland, so he could make sure that new data and ideas would not languish in unread academic papers. He wanted to directly influence the construction of the next generation of hospitals. With Brown on board, Green persuaded the Sloan Foundation to put some start-up money behind a first-of-its-kind collaboration between architects and microbiologists.
The BioBE Center was born.
Fighting the Ick Factor
“Is nobody going to touch the pastries?” asks Jessica Green. “Come on!”
At the BioBE Center’s weekly Monday meeting, a full box of bagels and Danishes sits on the conference table like an untold joke. Bring a bunch of microbiologists together, set food before them, and watch them wonder what kind of microscopic menagerie is scuttling around the raisins and sugar glaze. Brendan Bohannan cracks wise. “Maybe we’re still full from that mouthful of microbial yogurt that came out of the showerhead this morning.”
Mild amusement all around. In this room, Norman Pace’s study has attained a subcultural notoriety. Physicists joke about the Higgs boson particle; microbiologists riff on Pace’s showerhead slime. It’s not all microbiologists here, of course. Sitting around the table are evolutionary ecologists, energy physicists, and architects. “Part of BioBE is simply learning to speak each other’s language,” Bohannan says.
Charlie Brown, the architect, pipes up. “In their microbiology studies, they’ll often report that they sampled ‘a room’ or ‘a classroom.’ What? That means nothing to someone working in the built environment. Give us dimensions! Windows, doors, airflow, temperature, materials.” To that end, the BioBE Center’s microbiologists have begun working on more rigorous ways to sample the air and various surfaces of their two test buildings, the Lillis Complex and Providence Milwaukie Hospital in a suburb of Portland.
Steven Kembel, a research biologist, shows the team his latest microbial sampler. It looks like a plastic document box with a microphone sticking out of it. The microphone is actually a filter-tipped vacuum. Its big advantage over current devices is not accuracy but unobtrusiveness. “We need to sample the air in rooms where people are studying and lecturing,” Kembel says. “If the Shop-Vac motor is too loud, they just throw the box out of the room.” So he packed his latest model with noise-muffling foam. He clicks a switch and it runs at a low brrr. Green nods her approval. “Sampling a building makes people uncomfortable,” she says. “They’re afraid of what you might find.” Kembel’s quiet air sampler should open more doors to her researchers.
“We call it the ick factor,” Bohannan explains to me. “It’s something we’re constantly having to overcome.”
Speaking of ick: Jeff Kline, a forensic architect, follows with a slide show of the Lillis Complex’s unique ventilation system. The classrooms are stair-stepped, like an amphitheater, and ducts between the risers allow outside air to flow into the building. Kline displays an under-the-floor photograph revealing a filthy duct full of candy wrappers, pens, paper, and dust drifts. The microbiologists perk up. They love dust. “Dust is a historical record of all that’s lived there,” Bohannan says. Looking at the dirty floor in Kline’s photo, he says, “Behold the Burgess Shale of microbiology.”
Next up in the meeting, Kembel wonders if the presence of humans in a room affects which microbes flourish and which die out. Green mentions a recent study by bioengineer Jordan Peccia at Yale, who sampled microbes in a Yale Law School classroom. When it was unoccupied, microbes settled out of the air onto the floor, desks, and walls. When people entered, they acted like tornadoes, resuspending those settled microbes. “And we still have a lot to learn about the microbes we’re contributing ourselves by being in the room,” she says.
“Right,” Bohannan adds. “How much we flux from our bodies.”
I ask for a clarification. “Flux—you mean shed? Slough from our skin?”
Bohannan smiles. “I prefer flux,” he says. “It’s a less value-laden term.”
This year the BioBE team will start testing that human microbial flux in a chamber now under construction in a Portland office building. A giant clean room with more than 150 installed sampling devices, it will give scientists the ability to precisely control temperature, airflow, humidity, and other variables. Once it is running, the team will be able to determine how many and what kind of microbes humans contribute to the indoor environment. “We know more about soil microbes than we do about those on our own body,” Bohannan says.
As the meeting breaks up, one of the microbiologists takes a bagel. Others follow her lead. Hunger overcomes the ick factor.
Next Page: The Microbe-Friendly Hospital
The Microbe-Friendly Hospital
Later that morning, Charlie Brown walks me through some computer modeling he is doing on hospital rooms, ventilation, and windows. “In most buildings now, the problem isn’t heating, it’s cooling,” he says. New buildings are so tightly sealed and energy efficient that very little warmth escapes—but inside, human bodies and office equipment radiate plumes of heat. Brown wants to figure out how to use more natural ventilation to cool hospitals and reduce their energy footprint. It is a modern take on an old idea. “The want of fresh air may be detected in the appearance of patients sooner than any other want,” Florence Nightingale wrote in her 1859 Notes on Hospitals. Nightingale championed the restorative effects of outdoor air received through open windows. “To shut up your patients tight in artificially warmed air,” she warned, “is to bake them in a slow oven.”
From the 1870s through the 1940s, when tuberculosis was raging across Europe and the Americas, TB patients were sent to sanatoriums where they were prescribed rest and plenty of fresh air. In the 1950s new anti-tubercular drugs put sanatoriums out of business. In the 1970s architects began incorporating HVAC systems into new hospital design. To work properly, those systems required complete control of indoor airflow. The result: sealed windows. Who would want to open a window when HVAC ducts delivered perfectly regulated air? “The idea of fresh air became disconnected from the way we design and build hospitals,” Kembel says. Architects thought only of temperature and air exchange rates. They did not consider that outside air might actually contain properties—namely diverse and beneficial microbes—that could make it healthier than inside air.
Nightingale’s belief in the healthy properties of fresh air was revived in 2007 by British researcher Rod Escombe. He noted that tuberculosis was still a global killer, causing 1.8 million deaths every year. Most of those cases occurred in developing countries, where TB infection is often spread by patients coughing in poorly ventilated hospitals. In a series of studies at hospitals in Lima, Peru, Escombe showed that the simple act of opening windows could cut the risk of TB infection by two-thirds.
That finding led the BioBE researchers to ask a basic question: Just how different is outside air from inside air? “We wanted to know what happened to outdoor microbes when they came in through the hospital window,” Kembel says. “And what happens to indoor microbes when you open a window? Until a couple of years ago we didn’t have the DNA tools to find out. Now we do.”
In 2011 the BioBE Center team sampled airborne bacteria in patient rooms at Providence Milwaukie Hospital. They studied the rooms with the windows closed and then opened. The team found 0.5 million to 2.5 million bacterial cells per cubic meter of air, which is about what they expected. But other data caught them off guard. “I didn’t expect to see such a dramatic difference between indoor and outdoor air,” Green tells me in her office. Indoor and outdoor air contained almost completely different microbial species. The outside air held mostly bacteria found in soil, water, and leaf surfaces. Most of the airborne bacteria in the closed-window room was specific to the human biome—the bacteria that we shed from our skin, hair, and mouths.
“It’s extraordinary to me that we’ve come almost full circle,” Green continues. “Having reached a point where we’re doing exactly the opposite of what Florence Nightingale advocated 150 years ago, designing hospitals that are shut up tight, we’re now turning up scientific data that confirm her theories.” The take-home message is clear: Sealing up a building makes the indoor environment look a lot more human. “And that’s not necessarily a good thing,” Green says.
That still leaves the BioBE team with basic questions about why hospitals are so dangerous. Does the hospital ecosystem encourage dangerous microbes to flourish? Or do harmful microbes exist in all buildings, and hospitals merely attract a human population that is particularly susceptible to them? If it is the former, Green wants to find a way to create a healthier microbial ecosystem, not chase after the bad organisms one by one. That may lead to radical new floor plans, ventilation systems, and ways to bring healthy outside microbes inside. “There’s a beautiful biology going on in buildings,” she says. “We’ve got to understand ecology and evolution if we want to manage the indoor environment.”
From there, Green adds, it is just a matter of scaling up. “Once you think about rooms and buildings as ecological environments, you’re really talking about island biogeography.” For Green, rooms are islands and the building is an archipelago. “Think of the air like the sea around those islands. It’s connecting the islands through corridors and the mechanical ventilation system. People are dispersal agents, moving from space to space. It’s all happening there. Everything we’ve learned about outdoor environments happens indoors, too: random birth and death events, competition for resources, and coevolution of different organisms.”
As Green concludes, the HVAC system clicks on. Filtered air pushes through a vent in her office wall. I turn to leave, disturbing a cloud of microorganisms at my feet.
Mapping the Home's Microbe Habitats
Most studies of microbes in the home have focused on a particular location, such as the shower curtain or the hot-water heater. Now North Carolina State ecologist Rob Dunn aims to survey what’s living on everything—from pillowcases to refrigerators—in thousands of U.S. residences.
Last fall Dunn began his “Wildlife of Our Homes” project with a pilot study in which 40 volunteers swabbed eight locations in their houses and mailed back the samples. He then had a lab sequence and analyze the DNA of the microbes, fungi, and other creatures captured on the swabs. The study yielded fascinating, if somewhat unpleasant, revelations. “The pillowcase and the toilet seat actually have a lot in common,” says Holly Menninger, the project’s director of public science. In fact, there is so much overlap between the bacterial strains in those two locations that it can be difficult to tell where a particular sample came from. The similarity isn’t entirely surprising, since the microbes in both places are most commonly associated with human bodies. Among the hundreds of strains present on pillows and toilets are bacteria from the Staphylococcus and Streptococcus families, which typically live on the skin. There are also plenty of gut microbes in both places (which means that the pillows were seeded with what scientists delicately refer to as “fecal contamination”). Dunn and his team are finding consistent patterns across the houses they have sampled so far. The toilet seat and the pillowcase always have a lot in common. Less disturbing, the kitchen counter populations overlap with those on the cutting board and the fridge, all of them dominated by bacteria found on produce. The interior and exterior doorsills of the house also share bacterial populations—mainly strains that are found in soil and blow around in dust.
In his preliminary data, Dunn sees each home as a diverse mixture of ecosystems, almost a planet in miniature. “These are predictable habitats,” he says. “We’re essentially finding the deserts and rainforests of houses.” —Veronique Greenwood
Bugs in Space
Astronauts come and go at the International Space Station, but for the untold billions of microbes that have hitched a ride into orbit, it is home. In a project called SWAB (Surface, Water, and Air Biocharacterization), NASA microbiologists keep tabs on the station’s microscopic residents by sampling the water crew members drink, the air they breathe, and the surfaces they touch. SWAB is primarily aimed at keeping pathogens in check, but it also monitors how the onboard microbial ecology changes over time. “The ISS essentially gets reinoculated whenever a craft docks,” says NASA microbiologist Duane Pierson.
The team is finding that the populations are not the only things that change; space travel alters the microbes themselves. Arizona State University biologist Cheryl Nickerson recently discovered that Salmonella becomes several times more virulent in space, a transformation that disappears within hours of the bacterium’s return to terra firma. The microgravity environment might alter how Salmonella’s genes are expressed, raising the prospect that other microbes could also become more dangerous in space than they are on Earth. —Sophia Li
Bruce Barcott is the author of The Last Flight of the Scarlet Macaw. He writes on science and the environment for National Geographic, Outside, On Earth, and other publications.