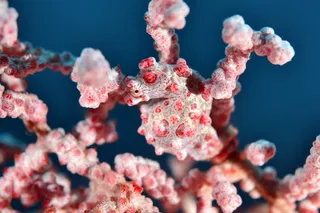
Introduced bee on a native ʻōhiʻa flower. Photo by Flickr user Zesuri As most of my friends on the mainland don longer sleeves and more layers, it's hard not to be a little smug about living in paradise. While, in their neighborhoods, leaves are falling off of trees and icy winds threaten to bring snow, I can throw on a T-shirt and shorts, grab a picnic basket, and hike to a scenic overlook for lunch. But Hawaii's ever-sunny weather comes with one side-effect that can be deadly serious: year-round, Hawaii has bees. Don't get me wrong—bees are wonderful insects, even though most species are not native here in Hawaii. When the first Hawaiians arrived on the shores of these stunning isles, only the yellow-faced bees buzzed around. Honey bees were introduced in the 1850s, and have since become indispensable, wedging their way into the Hawaiian economy and filling the shoes ...
Did Allergies Evolve To Save Your Life?
Bee allergies pose a serious risk for millions, potentially leading to anaphylactic shock. Understanding the adaptive immune response is crucial.
More on Discover
Stay Curious
SubscribeTo The Magazine
Save up to 40% off the cover price when you subscribe to Discover magazine.
Subscribe