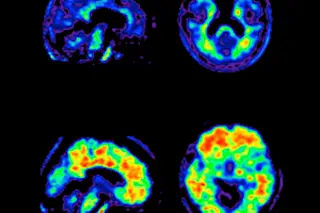
Part of what makes Alzheimer’s disease so pernicious is its stealth. Traditionally, it could be identified with certainty only by an autopsy. That changed last year, when researchers used two tools to diagnose the disease with nearly 100 percent accuracy in living subjects, a feat that might ultimately allow patients to seek drug treatment before their condition becomes too advanced.
In the first method, doctors inject a radioactive dye that binds to amyloid plaque, a damaging protein that accumulates in patients’ brains and is the hallmark of the disease; then they detect the dye with a pet scan of the brain. Last summer researchers at Avid Radiopharmaceuticals in Philadelphia used the technique to identify 34 of 35 Alzheimer’s patients, as later confirmed by autopsy. Given that 20 percent of people currently diagnosed with Alzheimer’s turn out to be suffering from something else—notably depression, B12 deficiency, Parkinson’s dementia, or vascular disease ...