A simple difference in the genetic code – two X chromosomes versus one X chromosome and one Y chromosome – can lead to major differences in heart disease. It turns out that these genetic differences influence more than just sex organs and sex assigned at birth – they fundamentally alter the way cardiovascular disease develops and presents.
While sex influences the mechanisms behind how cardiovascular disease develops, gender plays a role in how healthcare providers recognize and manage it. Sex refers to biological characteristics such as genetics, hormones, anatomy, and physiology, while gender refers to social, psychological, and cultural constructs. Women are more likely to die after a first heart attack or stroke than men. Women are also more likely to have additional or different heart attack symptoms that go beyond chest pain, such as nausea, jaw pain, dizziness, and fatigue. It is often difficult to fully disentangle the influences of sex on cardiovascular disease outcomes versus the influences of gender.
While women who haven’t entered menopause have a lower risk of cardiovascular disease than men, their cardiovascular risk accelerates dramatically after menopause. In addition, if a woman has Type 2 diabetes, her risk of heart attack accelerates to be equivalent to that of men, even if the woman with diabetes has not yet gone through menopause. Further data is needed to better understand differences in cardiovascular disease risk among nonbinary and transgender patients.
Despite these differences, one key thing is the same: Heart attack, stroke, and other forms of cardiovascular disease are the leading cause of death for all people, regardless of sex or gender.
We are researchers who study women’s healthand the way cardiovascular disease develops and presents differently in women and men. Our work has identified a crucial need to update medical guidelines with more sex-specific approaches to diagnosis and treatment in order to improve health outcomes for all.
Gender Differences in Heart Disease
The reasons behind sex and gender differences in cardiovascular disease are not completely known. Nor are the distinct biological effects of sex, such as hormonal and genetic factors, versus gender, such as social, cultural and psychological factors, clearly differentiated.
What researchers do know is that the accumulated evidence of what good heart care should look like for women compared with men has as many holes in it as Swiss cheese. Medical evidence for treating cardiovascular disease often comes from trials that excluded women since women, for the most part, weren’t included in scientific research until the NIH Revitalization Act of 1993. For example, current guidelines to treat cardiovascular risk factors such as high blood pressure are based primarily on data from men. This is despite evidence that differences in the way that cardiovascular disease develops leads women to experience cardiovascular disease differently.

(Credit: FG Trade Latin/E+ via Getty Images) Gender biases in health care influence the kind of tests and attention that women receive.
FG Trade Latin/E+ via Getty Images
In addition to sex differences, implicit gender biases among providers and gendered social norms among patients lead clinicians to underestimate the risk of cardiac events in women compared with men. These biases play a role in why women are more likely than men to die from cardiac events. For example, for patients with symptoms that are borderline for cardiovascular disease, clinicians tend to be more aggressive in ordering artery imaging for men than for women. One study linked this tendency to order less aggressive tests for women partly to a gender bias that men are more open than women to taking risks.
In a study of about 3,000 patients with a recent heart attack, women were less likely than men to think that their heart attack symptoms were due to a heart condition. Additionally, most women do not know that cardiovascular disease is the No. 1 cause of death among women. Overall, women’s misperceptions of their own risk may hold them back from getting a doctor to check out possible symptoms of a heart attack or stroke.
These issues are further exacerbated for women of color. Lack of access to health care and additional challenges drive health disparities among underrepresented racial and ethnic minority populations.
Sex Difference in Heart Disease
Cardiovascular disease physically looks different for women and men, specifically in the plaque buildup on artery walls that contributes to illness.
Women have fewer cholesterol crystals and fewer calcium deposits in their artery plaque than men do. Physiological differences in the smallest blood vessels feeding the heart also play a role in cardiovascular outcomes.
Women are more likely than men to have cardiovascular disease that presents as multiple narrowed arteries that are not fully “clogged,” resulting in chest pain because blood flow can’t ratchet up enough to meet higher oxygen demands with exercise, much like a low-flow showerhead. When chest pain presents in this way, doctors call this condition ischemia and no obstructive coronary arteries. In comparison, men are more likely to have a “clogged” artery in a concentrated area that can be opened up with a stent or with cardiac bypass surgery. Options for multiple narrowed arteries have lagged behind treatment options for typical “clogged” arteries, which puts women at a disadvantage.
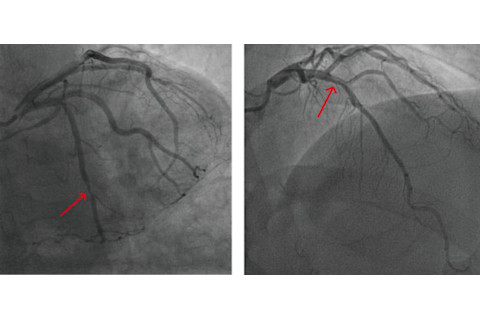
(Credit: Zhao and Gong 2023/Mathematical Biosciences and Engineering) Blood vessels don’t need to be clogged by plaque to cause heart disease.
Zhao and Gong 2023/Mathematical Biosciences and Engineering
In addition, in the early stages of a heart attack, the levels of blood markers that indicate damage to the heart are lowerin women than in men. This can lead to more missed diagnoses of coronary artery disease in women compared with men.
The reasons for these differences are not fully clear. Some potential factors include differences in artery plaque composition that make men’s plaque more likely to rupture or burst and women’s plaque more likely to erode. Women also have lower heart mass and smaller arteries than men, even after taking body size into consideration.
Reducing Sex Disparities
Too often, women with symptoms of cardiovascular disease are sent away from doctor’s offices because of gender biases that “women don’t get heart disease.”
Considering how symptoms of cardiovascular disease vary by sex and gender could help doctors better care for all patients.
One way that the rubber is meeting the road is with regard to better approaches to diagnosing heart attacks for women and men. Specifically, when diagnosing heart attacks, using sex-specific cutoffs for blood tests that measure heart damage – called high-sensitivity troponin tests– can improve their accuracy, decreasing missed diagnoses, or false negatives, in women while also decreasing overdiagnoses, or false positives, in men.
Our research laboratory’s leaders, collaborators, and other internationally recognized research colleagues – some of whom partner with our Ludeman Family Center for Women’s Health Research on the University of Colorado Anschutz Medical Campus – will continue this important work to close this gap between the sexes in health care. Research in this field is critical to shine a light on ways clinicians can better address sex-specific symptoms and to bring forward more tailored treatments.
The Biden administration’s recent executive order to advance women’s health research is paving the way for research to go beyond just understanding what causes sex differences in cardiovascular disease. Developing and testing right-sized approaches to care for each patient can help achieve better health for all.
Amy Huebschmann is a Professor of Medicine at the University of Colorado Anschutz Medical Campus. Judith Regensteiner is a Professor of Medicine at the University of Colorado Anschutz Medical Campus. This article is republished from The Conversation under a Creative Commons license. Read the original article.