Our first patient in the gastroenterology clinic one morning was a 68-year-old retired cafeteria worker with vague abdominal pains. Basic blood tests and an endoscopic examination of her digestive tract turned up nothing, so she was referred to me for further evaluation. The pains in her midabdomen came and went, sometimes radiated to other areas, and were often triggered by meals. Some days she had no pain. She often felt better when fasting or after a bowel movement.
My first thought was that the patient might have irritable bowel syndrome, a condition that is associated with intermittent abdominal pain in the absence of any visible abnormality. But it would be unusual for it to turn up for the first time in a woman this age.
I noticed that the patient was quite thin, 5 feet 4 inches tall and only 100 pounds. When I asked her if she had lost any weight, she simply shrugged and told me she didn't even own a scale. I asked to look at the photo on her driver's license for comparison, and she did appear to have shed some pounds. Still, when I performed a physical examination, she seemed healthy.
Her chart showed that she was taking an oral medication to lower the level of glucose in the blood. I asked her if she was diabetic.
"Yes, I am," she replied. "It was just diagnosed a few months ago, much to my surprise."
"Why were you surprised by the diagnosis?" I asked.
"I never had problems with my blood sugar until now," she said. "Plus, nobody in my family has diabetes, so I guess I was just the lucky one. Now they tell me I have to take these medicines forever, and I hate checking my blood sugar all day long!"
The fact that she had new-onset diabetes raised a red flag for me, especially because she was so thin. Diabetes that develops after childhood is often a disease of overweight individuals who have become resistant to insulin, the hormone the pancreas secretes to lower the level of glucose in the bloodstream. This type of diabetes is uncommon in thin people.
"Does the pain in your stomach ever radiate through to your back?" I asked.
"Yes, yes, it does," she said after thinking for a moment. "Sometimes when I lie down at night."
"We need to take a look in your belly and make sure your pancreas is OK," I told her. "I'll order a CT scan of your abdomen right away."
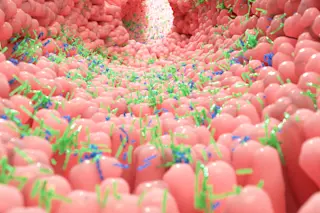
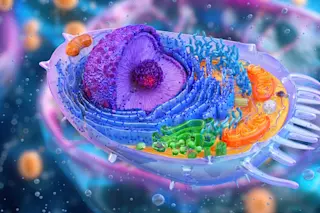
The pancreas, which sits behind the stomach and in front of the spine, is a woefully misunderstood organ. Most of us think that the stomach is the main digestive organ, but in fact it does only a small part of the job. The pancreas secretes enzymes that break down foods into their basic building blocks. These simple sugars, fats, and peptides are then absorbed by the small intestine, whereas the colon primarily absorbs water. Most people are blissfully unaware of the pancreas until it gets them into trouble, usually by becoming inflamed, a condition known as pancreatitis, or by turning cancerous.
Vague abdominal pains are a dime a dozen, but vague abdominal pains in the presence of new-onset diabetes raise the possibility of pancreatic cancer. In addition, abdominal pain that radiates to the back often suggests a problem in the pancreas itself.
Despite intense investigation over the past decade, the relationship between diabetes and pancreatic cancer remains poorly understood. Many patients with pancreatic cancer develop high blood sugar, or hyperglycemia, which can progress to full-fledged diabetes. The reasons for this remain unknown. One hypothesis is that tumors of the pancreas destroy enough of the insulin-producing islet cells in the pancreas to cause diabetes. Another possibility is that pancreatic tumors somehow make patients become insensitive to insulin. The basis for this hypothesis is that patients often regain sensitivity to insulin following the removal of the tumor.
Some physicians have advocated studying patients with new-onset diabetes as a population at high risk for pancreatic cancer. They have proposed screening these patients with special blood tests, ultrasound exams, and CT scans. However, there are reasons to be cautious. More than 1 million new cases of diabetes are diagnosed in the United States each year, but pancreatic cancer is comparatively rare, with only about 30,000 new cases in the United States during the same period of time. Testing everyone who developed diabetes in hopes of finding a small number of patients with pancreatic cancer would be prohibitively costly.
Still, if the diabetes leads to the discovery of the cancer (and not the other way around), the cancer is more likely to be at a stage at which it can be successfully removed. Understanding this possibility is especially important because the overwhelming majority of patients have their pancreatic cancer diagnosed when the cancer has become incurable. Most patients die within six months of diagnosis. Usually the tumor has already spread to another organ, or the primary tumor has wrapped itself around one of the nearby major abdominal arteries, making surgical removal of the tumor too risky.
Later that day I got the results of the patient's CT scan. It showed fullness in her pancreas that could be a tumor. She was hospitalized for further testing.
The next morning, I performed an endoscopic ultrasound. After the patient was sedated, I inserted an endoscope with a tiny built-in ultrasound instrument through her mouth and into her stomach and intestines. The ultrasound let me look through the wall of her stomach and small intestine and see her pancreas in exquisite detail. What had appeared as fullness on the CT scan looked like a classic pancreatic cancer. To confirm the diagnosis, I inserted a needle through the endoscope to take a biopsy from the core of the mass. A pathologist standing by examined the tissue and verified that the cells from the mass were cancerous.
The tumor was surgically removed the following week.
My patient was lucky. If she had waited a few more months to get medical attention, she might have died from inoperable pancreatic cancer.
The relationship between diabetes and pancreatic cancer is still being explored, and doctors must rely on their clinical judgment and experience when deciding which patients with new-onset diabetes should be screened for pancreatic cancer. Yet, given how few tools exist for discovering patients with pancreatic cancer early in the course of the illness, any new way to identify potentially curable patients is a source of hope.
Douglas G. Adler is assistant professor of medicine at the University of Texas Medical School at Houston. The cases described in Vital Signs are true stories, but the authors have changed some details about the patients to protect their privacy.