Editor’s Note: Tony Dajer has practiced emergency medicine for 25 years in New York City. He’s a frequent physician-writer for Discover’s popular medical mystery column, Vital Signs. Here, he writes about three of his recent ER patients, and what that might say about COVID-19’s effects on the heart.
180. Room 5.
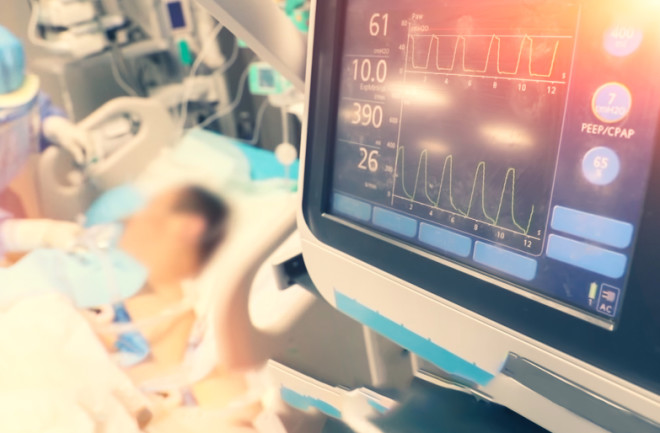
The red digits glared from the central monitor. Was the new patient’s heart rate really 180 beats per minute? Twice normal, a pulse of 180 usually signifies a patient in extremis. But no one was running: not the residents, not the nurses. I glided over. The 62-year-old man in room 5 looked surprisingly OK. The monitor flashed a normal blood pressure and oxygen saturation.