Guess who’s in the waiting room? the charge nurse sings out in a high-pitched voice as she walks into the emergency department. Without waiting for our guesses, she answers herself: Livinia!
A chorus of doctors’ and nurses’ voices erupts from the work station.
Her again?
What a wimp.
But I just saw her here two weeks ago.
Oh, no--not Livinia!
I’ll admit it--this is unbecoming conduct for health professionals talking about a patient, particularly one with a serious chronic disease. And if you were to meet the person whose presence provoked this outburst, you’d be even more appalled. Livinia Johnson is a perfectly pleasant, well-mannered and well-dressed 29-year-old black woman who works as a computer programmer and is a voracious reader of science fiction in her spare time.
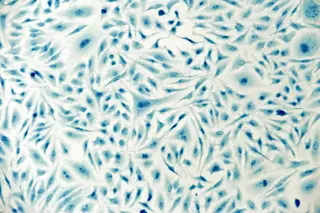
But Livinia Johnson also suffers severe recurring bouts of pain from the distressingly common and untreatable condition called sickle-cell anemia. As she’s ...