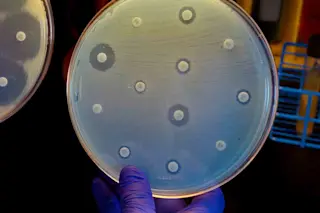
For years, United States public health officials have watched nervously as drug-resistant superbugs marched around the world, killing hundreds of thousands of people. Then in January, a report from the Centers for Disease Control and Prevention revealed that an elderly Nevada woman had died of a bacterial infection that defied even the biggest guns in the infection-fighting arsenal. That’s when many U.S. experts sounded the alarm: Time is running out to stop these deadly pathogens.
“We’re somewhere between total panic and a situation we feel confident we can manage,” says James Johnson, a professor of medicine and infectious diseases at the University of Minnesota. Already, superbugs claim 23,000 American lives every year, and over the past eight years, the number of hospitalized children who are resistant to antibiotics has increased sevenfold.
Globally, the situation is much worse: More than 700,000 die annually from drug-resistant infections, particularly in parts of Europe, ...