I peeked into the emergency room cubicle as our nurse manager filled me in. “Fifty-two-year-old. Sudden nausea and weakness. Blood pressure’s low: 66 over 40. Only history is obesity surgery four years ago.” Vincent, my fellow attending, stood at the bedside. Mr. Dexter, the patient, was alert and uncomplaining.
“Can’t be too sick. Probably vasovagal,” I thought, walking on. The vasovagal reaction is a catchall term for a transient condition involving fear or pain, such as gastrointestinal upset, that causes low blood pressure, slow heart rate, and in some cases fainting. Patients who have had gastric bypass surgery, a treatment for obesity that dramatically reduces the size of the stomach, often experience such upset. The condition usually passes quickly.
An hour later, Vincent buttonholed me. “Could you help me look at his heart?” he asked. “We’ve given three liters of saline, plus dopamine [a blood pressure booster]. Blood pressure won’t come up. EKG shows no heart attack. No fever, headache, chest pain, or abdominal pain,” he added. “Maybe the ventricle wall isn’t contracting right. EKGs don’t always pick up heart attacks.”
The numbers on the monitor jolted me: still 66 over 40. So much for my snap diagnosis.
I wheeled the ultrasound machine over.
“What does that do, doctor?”
“We’re going to look at your heart,” I told Mr. Dexter. “No chest pain, right?”
“That’s correct, doctor.”
“Tell me again what happened.”
“I was sitting at my desk,” he related. “A wave of weakness hit me, then I got short
of breath. Nausea, too.”
“No pain anywhere?”
“Not that I can recall.”
His heart looked fine. He didn’t have fever, vomiting, or diarrhea.
In medical parlance, a drop in blood pressure is known as shock. It has nothing to do with emotional upset and everything to do with hydraulics. When blood pressure suddenly dips, there are three main possible causes: pump failure (as in a heart attack), leaky blood vessels (an immune response to an overwhelming infection), or fluid loss (bleeding or dehydration). A systolic pressure of 66 meant Mr. Dexter had lost about two quarts of blood. So where was it? The GI tract—the most common source of spontaneous hemorrhage—was clean.
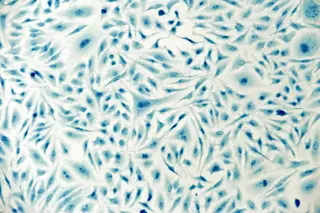
I placed the ultrasound probe on Mr. Dexter’s right flank, where the kidney and liver meet. Anatomists call this spot Morison’s pouch. Luckily for emergency room doctors, it’s easy to find and happens to be where free fluid in the abdomen accumulates. Immediately a broad black stripe showed up between the grayish-looking liver and the right kidney.
“Lots of free fluid in there,” I announced. An ultrasound cannot distinguish between blood and other fluids, but there was no reason for Mr. Dexter to have ascites, the accumulation of fluid in the belly that can come with cirrhosis of the liver.
“Do you have any belly pain?”
“You guys keep asking me that.”
“How about this?” I gently pressed a hand into his stomach.
“OK, OK that hurts some, but not bad.”
Blood can be highly irritating to the abdomen’s lining, so if the excess fluid was blood, Mr. Dexter should have felt more pain, but following gastric bypass surgery, he no longer had a normal abdomen.
With low blood pressure and possible blood in the belly, this patient was now an official emergency. “Call the surgeons—now!” I ordered. “Make sure he’s typed and crossed for four units.” More nurses swarmed in.
An intern entered, waving a slip of paper: “His hematocrit is 26.” That’s a low—but not critically low—red blood cell count.
“I’ve been a little anemic in the years since the surgery,” Mr. Dexter offered.
“What’s your usual level?” I asked.
“Don’t know. Sorry.”
Don, one of our surgeons, came charging down with his team. “Odd thing is,” I told him, “his belly’s not tender, but look at this.” I passed the ultrasound wand over the black band again.
“I see it,” Don said. “I believe you.”
“Could he have a PE?” the chief surgical resident mused, referring to a pulmonary embolus, or blood clot in the lung. “The gastric bypass puts him at risk. Or maybe a suture line eroded or there’s a perforation leaking stomach contents.”
The list of possibilities seemed endless. With no time to spare and Mr. Dexter too unstable to undergo a CT scan to image the lung, we would have to decide on an operation based on our own judgment.
“Why should a healthy man suddenly bleed into his belly?” Don asked. “And then not be tender? What if it’s a PE and we operate, then have to anticoagulate him? Nightmare.”
“His oxygen level’s not bad,” I said.
“It’s like he has half of everything,” the chief resident observed.
“How about we look at his heart with a bedside echocardiogram?” I suggested. “If the pulmonary artery is corked by a clot, we’ll see a dilated right ventricle.” Echocardiograms create images of a beating heart, to help doctors spot problems in cardiac structure and function. Mr. Dexter’s results were normal.
“We’ve wasted enough time. Let’s go,” Don ordered.
Suddenly the monitor beeped: Blood pressure was now 110 over 60. Mr. Dexter was in safer territory now.
I held Don back. “His blood pressure’s better. Maybe something clotted off. Why don’t we sneak a CT scan on the way up?”
Fifteen minutes later, everyone crowded into the radiology suite. The scan showed blood everywhere.
“What’s that?” Don tapped the lower pole of the spleen, where an odd lesion that resembled a bull’s-eye lay at the center of the bleeding. “Aneurysm? Tumor?”
“I don’t know,” the radiologist replied. “Never seen anything like it.”
“Guess there’s only one way to find out,” Don concluded.
What we saw suggested an aneurysm—a malformation of a blood vessel, an uncommon but devilish ailment. Most stem from genetically influenced defects in proteins of the arterial wall. Aneurysms, which bulge like a balloon squeezed too tightly, often arise at an artery’s branching point, though they can pop up anywhere. Until they burst without warning, they can escape diagnosis because the irritation caused by blood mimics that of a common infection or even a migraine. In adults 30 to 60 years old, aneurysms rupture most frequently in the brain, causing tens of thousands of fatal or disabling hemorrhages each year. Women are particularly vulnerable. The abdominal aorta, for its part, can bulge out and burst anywhere, but only rarely does this happen in someone under 55.
Then there are the odd ducks, like splenic artery aneurysms. The spleen lies under the left diaphragm, behind the ninth, tenth, and eleventh ribs. It’s like the body’s oil filter, trapping old red blood cells and certain types of bacteria and removing them from circulation. Unfortunately, the spleen’s good-size artery is at risk for an aneurysm during pregnancy, particularly in the third trimester, when the enlarging uterus presses on the vessel, increasing its blood pressure. I know of four cases of ruptured splenic artery aneurysms in pregnant women, each presenting as upper-abdominal pain and vomiting in the third trimester. Flummoxed doctors mistook them for stomach viruses—until the patients’ blood pressure plummeted. Two of the women died; the others were saved by last-minute surgery.
Don’t fret too much about your plumbing, though. We Homo sapiens are well-put-together organisms. Blowing a gasket is a rare event. However, given that the body will do everything possible to keep blood pressure up, a sudden drop should, in this age of bedside ultrasound, prompt a quick look at the plumbing. There is no easier way to save a life.
Three hours later, Don swung by the emergency room, digital camera in hand. “It was a bulge, like an aneurysm, where the artery enters the spleen,” he told me, clicking through photos of the crescent-shaped maroon organ. “Splenic peliosis. Ridiculously rare. Cause unknown. Good thing we had the CT scan. Getting through all the adhesions from the gastric bypass surgery was tough, but at least we knew where to go. Luckily for him, it had partly clotted.
“Oh, and you know why the belly wasn’t tender?” he continued. “Adhesions from the gastric bypass had stuck his intestines up against the abdominal wall, forcing the blood to the sides. So even with a belly full of blood, it seemed like a benign exam.”
“Whew,” I whistled. “Close one.”
Two days later, Mr. Dexter was holding court in the intensive care unit. “So, should I play the lottery, doctor? They tell me I’m a million-to-one shot,” he joked. He looked so healthy I wanted to click my heels.
“No need for that. We already won,” I told him. “You are the jackpot.”
Tony Dajer is director of emergency medicine at New York Downtown Hospital in Manhattan. The cases described in Vital Signs are real, but names and certain details have been changed.