Photograph by Grant Delin
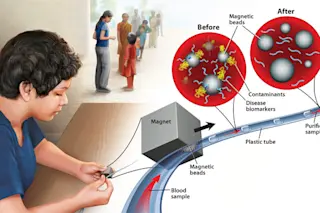
Scott Fischell, CFO and COO of NeuraLieve, tests a prototype of the company’s portable transcranial magnetic stimulator. The device sends magnetic pulses into the nerves of the head and cerebral cortex, stopping migraines cold.
Neil Hughes knows the sensation all too well. Everything goes blurry, and sunlight seems to reach his eyes bent every which way, as though he has suddenly slipped underwater. As the light grows brighter at the periphery of his field of vision, he raises his hands to cover his eyes, like the blinders on a horse. But the gesture is futile: An electrical firestorm, which medical researchers call an aura, is already raging inside his head.
Auras are neural disturbances that signal the onset of migraine headaches. They manifest themselves in numerous ways, including multichromatic showers of shooting stars, flashing lights, zigzagging lines, images broken up into herringbone or cubist patterns, loss of vision, weakness, tingling, or confusion. Sometimes the hallucinations mysteriously come and go and are a minor annoyance. More often, what follows is a nightmare: a seemingly interminable bout with throbbing head pain, nausea, and diarrhea.
For most of his adult life, Hughes, now 53, got migraines up to six times a month that rendered him violently ill, often with frightening spasms. “I would lose several days of my life lying in bed, not even knowing what time it was,” he says. He tried one remedy after another, to no avail. Doctors, he discovered, barely had a clue about what causes migraines and couldn’t offer him much relief. But now, after taking part in a clinical trial of a new device designed to quell the electrical storms in his brain, Hughes hopes he may never be laid low by a migraine again.
For the 40 million or so North Americans who suffer from chronic migraines, the condition has proved maddeningly resistant to treatment—or even explanation. Migraine researchers once focused most of their attention on the constriction and sudden dilation of blood vessels that serve the brain. They knew that stimuli such as bright lights, stress, chocolate, and other foods could trigger changes in cranial circulation. And they found that, in turn, hormonelike substances called prostaglandins were secreted along with other substances that, combined with the dilation of scalp arteries, stimulate the brain’s pain receptors. But that did little to explain what made one person rather than another a migraineur—someone who is prone to migraines.
In the early 1960s, researchers found that migraineurs produce low levels of serotonin, which inhibits pain and helps constrict blood vessels. This discovery led to the development of a class of drugs called triptans—most notably sumatriptan—that mimic the effect of serotonin. Triptans are still widely used and relieve active migraines 60 to 70 percent of the time. But they can also have dangerous side effects. When Hughes tried sumatriptan in the early 1990s, the injections set his heart racing and made him feel like his blood was on fire—“that’s how you knew it was working,” he says. He was willing to put up with the drug at first because it was so good at stopping migraines. Then he suffered two minor heart attacks. “My cardiologist said the drug could now kill me,” Hughes says. “So there I was, back to square one, living with Anacin.”
It wasn’t until the late 1990s that neuroscientists discovered a deeper source of migraines and their auras—and with it the potential for a cure. Migraineurs, they found, have a hypersensitive occipital cortex, which covers the back of the brain. By stimulating the cortical area responsible for vision, some researchers were able to trigger auralike hallucinations much more easily in migraineurs than in other subjects. The same sensitivity may make migraineurs more susceptible to bright lights, noise, and other triggers. Neuroimaging studies showed that such triggers set off an electrical wave of firing neurons that spread over the occipital cortex at a rate of several millimeters per minute. Known as a cortical spreading depression, this phenomenon had been hypothesized as far back as 1941 by the neuropsychologist and migraineur Karl Lashley. The unusual neuronal activity, in turn, seemed to foment the vessel dilation and release of prostaglandins and other substances first noted by migraine researchers.
Cortical spreading depression has also been observed in epileptics just prior to seizures, and this insight eventually led to the new migraine treatment Hughes has tested. Adrian Upton, a neurologist at McMaster University Medical Centre in Ontario, first suggested the idea in 2000. Upton had previously worked with the company NeuroPace—founded by the inventor Robert Fischell and his sons David, a physicist, Tim, a cardiologist, and Scott, an M.B.A.—to develop an implantable brain defibrillator for epileptics. By making neurons fire ahead of the cortical spreading depression, as if setting off a prescribed burn in the path of a forest fire, they found they could stop the wave of neurons from spreading, and thereby prevent seizures. “Why wouldn’t the same principle work on migraines?” they wondered.
When Upton asked Neil Hughes if he would participate in a clinical trial of the new treatment, Hughes agreed immediately. “Believe me,” he says, “I had nothing to lose.” Soon afterward, Hughes had one of his usual stupefying migraines, and his wife drove him to the McMaster medical center. There, a technician sat him next to a box the size of a desktop computer with a wire leading to what looked like a futuristic flyswatter. The device, known as a transcranial magnetic stimulator, is designed to send a strong electric current through a metal coil, which creates an intense magnetic field for about one millisecond. When held against a person’s head, that magnetic pulse creates an electric current in the nerves of the head and the neurons of the cerebral cortex, forcing them to fire prematurely. The stimulator had previously been used to treat depression, obsessive-compulsive disorder, and schizophrenia, in addition to epilepsy. But it had never been used on a migraine before, and Upton had no idea if it would work.
Upton held the magnetic stimulator next to Hughes’s head and pressed a button, sending out two pulses five seconds apart. Hughes says he felt a “surge, like a rush of energy” entering his head. Minutes later, after a second round, the headache was gone. No more pain, no more agonizing sensitivity to light when the blinds were opened. “It was amazing,” Hughes says. “Like a flood of release of the pain and pressure. You’ve no idea unless you’ve had migraines. I even drove home.”
In Upton’s clinical trials, three-quarters of all test subjects who arrived at the hospital suffering from a migraine reported feeling much better immediately after treatment. Better yet, every one of Upton’s subjects who has made it to the hospital during the aura phase has found that the magnetic stimulator dispels the aura and prevents the headache from occurring. Migraine drugs all have some side effects, including nausea, chest discomfort, and sometimes rebound headaches. But no side effects have yet been detected as a result of using the stimulator. In fact, Upton says, if the cycle of headaches—or seizures, for epileptics—is broken, then the patient may “forget” the pattern of electrical activity that leads to the symptoms. Since Hughes’s first three treatments, he hasn’t had a migraine in three years.
Other new migraine treatments have come along in the meantime. A biotech company called Capnia has developed a nasal spray that shoots concentrated carbon dioxide into the sinuses, where it interrupts cortical spreading depression by irritating nerve endings that lead to the brain. Clinical results have been encouraging. Topamax, an epilepsy drug from Ortho-McNeil Pharmaceutical, has proven extremely effective on migraines in clinical trials: Half of all patients have reported a 50 percent reduction in the frequency of migraines, and more than a quarter have a reported 75 percent reduction.
But the magnetic stimulator, thanks to its simplicity and lack of side effects, may prove to be the treatment of choice. A spin-off of NeuroPace, called NeuraLieve, is developing a lightweight handheld stimulator that migraineurs can carry around with them like a very large bottle of aspirin. The device, which weighs 2.5 pounds and runs on six AA batteries, will be in clinical trials by year’s end. “It looks a bit like a gun,” Scott Fischell admits with a laugh. “But I don’t think that matters too much. People will do anything to get rid of a migraine.”

The Roman emperor Justinian sought migraine relief in Istanbul by pressing his head to a “magical” pillar called the column of tears. Later sufferers were purged or bled, or their heads were encircled with a noose. One ninth-century headache tonic contained elderseed, cow’s brain, and goat’s dung in vinegar.
Discuss this article in the Discover Forum