When 5-year-old Jonathan Alava complained about stomach pains one day in February 2012, his mother, Shinna, laid him on the couch and rubbed his tummy. Only the flu, she figured; another preschool bug. Then she felt the hard lump, immediately knowing it didn’t belong and dreading its meaning. Diagnosis: a malignant tumor 10 centimeters wide, the size of a small grapefruit.
For more than 10 months, the child’s journey followed the kind of dreary, double-edged protocol so familiar to cancer patients and their families. The blunt weapons against cancer tend to be both helpful and harmful, especially in children. First came relentless weeks of chemotherapy to reduce the mass — enveloped, in Jonathan’s case, in a tangle of blood vessels doctors dared not disrupt with surgical tools. Chemo is a toxic brew that destroys microscopic metastases, errant cancer cells that have spread throughout the body, along with many healthy ones. Vomiting became a regular part of Jonathan’s life.
Once the tumor was reduced to the size of a walnut, a surgeon could move in and remove the mass. But it had attached to Jonathan’s bladder, abdominal muscles and the iliac artery, a major thoroughfare for blood between the heart and the pelvis. Worse, after a biopsy, specialists spotted an even more disconcerting complication lurking at the edge of the pathology specimen: stray cancer cells. They would have to use radiation on the preschooler.
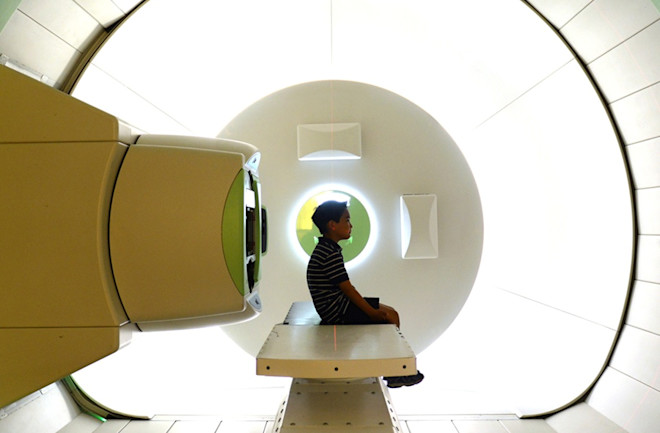
That’s when doctors say Jonathan got lucky. He had access to one of the most precise and powerful weapons in the modern anti-cancer arsenal, born out of regret after the bombings of Hiroshima and Nagasaki: a massive particle accelerator. Once exclusively the tool of physicists seeking to unravel mysteries smaller than the atom, the cyclotron has become the world’s most complicated and costly medical device. The machine, increasingly popular since it was introduced at a California medical center nearly 25 years ago, typically is as heavy as an airliner, surrounded by a shield of concrete and often housed in a building several stories tall. It delivers a straight, narrow beam of radiation that deposits most of its energy on the target tumor. Inflicting less collateral damage to surrounding organs and healthy tissues, it can minimize side effects and increase cure rates for some cancers — just what patients with small bodies like Jonathan need.