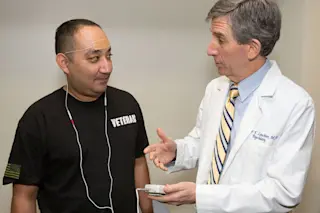
Ron Ramirez, a retired Army sergeant is participating in the second phase study investigating the effectiveness of external trigeminal nerve stimulation for veterans with PTSD. Andrew Leuchter is conducting the research as at UCLA's Semel Institute for Neuroscience and Human Behavior. (Credit: Reed Hutchinson/CalFoto/UCLA) Millions of people are suffering from post-traumatic stress disorder (PTSD) right now. Among military personnel who've been deployed to Iraq and Afghanistan, an estimated 31 percent are PTSD sufferers. An estimated 52 percent of people with PTSD also suffer from major depressive disorder (MDD). The cost of treating these disorders is estimated to run as high as $40 billion per year. The social consequences are harder to quantify, but many PTSD and MDD sufferers report marital problems, difficulties bonding with family and friends, and chronic suicidal thoughts. But a team of researchers led by Andrew Leuchter, professor of psychiatry and biobehavioral sciences at UCLA, believes it ...
Nerve Stimulation Offers Hope for PTSD Sufferers
Explore how external trigeminal nerve stimulation offers hope for veterans battling PTSD and MDD in a groundbreaking study.
More on Discover
Stay Curious
SubscribeTo The Magazine
Save up to 40% off the cover price when you subscribe to Discover magazine.
Subscribe