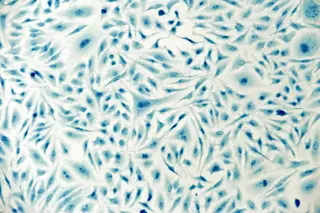
Liz Parrish is a CEO, humanitarian and patient zero in her own experiment. (Credit: BioViva) Elizabeth (Liz) Parrish is the CEO of BioViva, a biotechnology company that focuses on developing gene therapies, and other regenerative therapies, to intervene with human aging. Last September, Parrish added an interesting line to her job description: patient zero for two anti-aging therapies that the company is researching. Parrish is receiving two kinds of injections, which are administered outside the United States: a myostatin inhibitor, which is expected to prevent age-associated muscle loss; and a telomerase gene therapy, which is expected to lengthen telomeres, segments of DNA at the ends of chromosomes whose shortening is associated with aging and degenerative disease. The study will likely continue for many years. But last week, BioViva issued a press release describing an unexpected early result, offering a clue as to what the BioViva team might publish in the ...
Liz Parrish Is Patient Zero in Her Own Anti-Aging Experiment
Explore the potential of telomerase gene therapy with BioViva as Liz Parrish embarks on her groundbreaking anti-aging journey.
More on Discover
Stay Curious
SubscribeTo The Magazine
Save up to 40% off the cover price when you subscribe to Discover magazine.
Subscribe