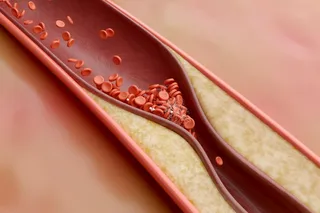
Jerry Silva's body was not designed for life in the early 21st century. A 44-year-old financial analyst from Sherborn, Massachusetts, Silva spends most of his time behind a desk tracking high-tech stocks. It's a life far removed from that of his Mexican forebears, who spent their days hoeing maize fields and fishing near Guadalajara. Silva has more than enough to eat, whereas his ancestors often went hungry. The significance of that difference in lifestyle became painfully apparent last January, when he was diagnosed with diabetes. The disease, closely linked with not eating the right foods and sitting around too much, is beginning to look something like a pandemic as millions of people around the world confront a central irony of the modern world: A lifestyle of abundance can be deadly.
On this planet 194 million people have diabetes, double the number of 25 years ago. In another 25 years the ...