The diagnosis appeared depressingly straightforward. The woman was 64. She had cervical cancer. And the X-ray I was looking at strongly suggested she would soon die from the disease.
But she didn't look like a terminal cancer patient. Sitting on the examining table at Cook County Hospital, Chicago's public hospital, this patient was ebullient, chatting along in Spanish with an Indian accent that I barely understood. She was round as a doughboy in her white paper gown, and her face, colored by the suns of Chihuahua, was deep brown. We had met a week ago when her daughter persuaded her to get her first Pap smear. A Pap smear is a sample of hundreds of thousands of cells scraped off the cervix, the lowermost end of the uterus, brushed onto a glass slide, and examined for abnormalities. The test is named after George Papanicolaou, who devised it for looking at hormonal function, then serendipitously found that the test detected cancer cells. Since the Pap smear was introduced in 1941, deaths from cervical cancer among American women have dropped by more than 70 percent.
The results of this patient's Pap smear had turned up cancer. The tumor was small, however, and I had told her that the disease appeared to be easily curable with radiation. She had laughed and held my hand and thanked God that I had been born. Then I sent her for other tests. Now I had the results, and when she saw my face, she grew serious and silent.
"Ay, Doctor," she said. "You look so serious. What happened?"
A routine evaluation of cervical cancer includes a chest X ray to see if the cancer has spread, or metastasized. Once cervical cancer spreads, therapy may be pointless because the outlook is so grim. This woman's X rays showed nodules in both lungs, as if someone had fired bird shot into her chest. The appearance was, as the radiologist reported, "suspicious for metastatic cervical cancer."
If the cancer reaches the lungs, especially in multiple nodules too numerous to remove surgically, patients die within months. Chemotherapy may shrink the nodules and may even cause them to disappear from the X ray, but the metastases always grow back from residual cells. Still, before giving up, I had seen a friend who is a pulmonologist. Together we came up with a diagnostic plan to find out if something else might be the cause of the lung nodules. As I explained this to my patient, she held out her hands, palms up.
"It's cancer or it's not, Doctorcito," she said, using the Spanish diminutive that meant she liked me even though I hadn't started to treat her. "You are the instrument of God in my life. I will do whatever you tell me."
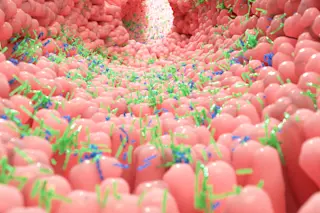
So we went through the tests. We collected sputum and analyzed it for tuberculosis, for fungi of the Sonoran Desert, and for cancer cells. We found nothing. A skin test for tuberculosis was negative. A scan of her chest showed myriad nodules, but they did not show the calcification or enlargement we expect to find from either conventional infections or the spread of cancer through the lymphatic system. Failure to find cancer with noninvasive tests doesn't mean it isn't there. The next step is a bronchoscopy. With this procedure, the pulmonologist sedates the patient and snakes a fiber-optic endoscope down the trachea and into the smaller airways. Saline is squirted into some of these passageways, then aspirated, or sucked back, and analyzed for pathogens and inflammatory cells that can sometimes produce nodules. If abnormalities are discovered in the airway, they can be biopsied. This part of the procedure is important for cancer patients because eroded areas in the walls of the airway can indicate that blood-borne cancer cells have become trapped in the lungs and are beginning to spread. In my patient's case, however, there were no tumors burrowing through the walls, and the test results for aspirated material were nonspecific. Still, to my friend, the results all made sense. There was no metastatic cancer. She had pneumoconiosis.
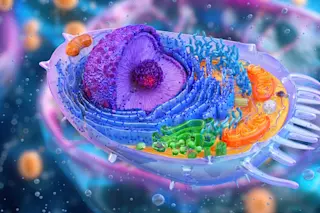
That diagnosis sent me first to my medical school texts, then to the Internet. The pneumoconioses are a grab bag of inflammatory lung diseases that develop in reaction to inhaled irritants. Small particles trapped in the lungs attract immune cells, which release enzymes and inflammatory molecules that cause scarring. Over time, with enough exposure to enough irritating particles, the scars become big enough to show up on chest X rays as nodules.
Perhaps the most common and best known pneumoconiosis in the United States is black lung disease, which coal miners develop from inhaling dust. Brown lung disease develops when cotton mill workers inhale tiny fragments of cotton-boll leaves. Asbestosis affects shipyard workers and others exposed to asbestos insulation. Inhalation of silica dust can cause silicosis among workers in sandblasting, quarrying, and stonecutting. And inhalation of the hardening agent beryllium can lead to berylliosis among those who manufacture alloys and ceramics. Occupational pneumoconioses used to be common among workers in these industries, but collaboration between industry, labor, and federal regulators in the United States has reduced—though by no means eliminated—their impact.
Even occupational exposure that occurred many years ago could not explain my patient's illness, because she had never worked outside her home. Still, there is another cause of pneumoconiosis that American physicians rarely encounter.
"Woodsmoke?" she replied when I began questioning her to confirm the pulmonologist's diagnosis. "Of course, I have been around woodsmoke." Her adobe house in northern Mexico had few windows, and in the winter the north wind blew smoke back down the chimney. Even in summer, she told me, she cooked her tortillas on stones over an open fire, as her mother, her grandmother, and all her relatives had done for generations.
There is no specific treatment for woodsmoke pneumoconiosis, or "hut lung," except to avoid the exposure. Rare in the United States, it is endemic in developing countries. Cases have been reported from Africa, southern Asia, and Latin America. It may be under-recognized in those countries because it is an occupational illness of women whose work is unpaid and undervalued. The pulmonologist and I told my patient that it was time to let her family cook for her on their gas range in the Chicago suburb where she had moved so she could spend her old age telling stories to her grandchildren. We treated her cancer with radiation for several weeks. These days she uses an inhaler to expand her scarred airways when she gets short of breath. She comes into the clinic every few months for her Pap smear, and she blesses me.
"You are the instrument of God, Doctorcito," she says, holding my hands in hers. It's a nice moment, and I sometimes wonder if she sees the lesson I learned: Nothing is ever as it seems.