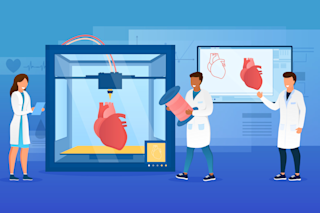
Each year desperately ill hospital patients—currently some 89,000 men, women, and children in the United States alone—languish waiting for a transplant of a liver, kidney, heart, or other essential organs. The doctors who attend them know there are not enough organs to go around. Many patients die waiting.
To improve those odds, tissue engineers are trying to harness the power of stem cells by designing three-dimensional plastic molds, called scaffolds or matrices, that resemble organs or body parts. When a soup of nutrients and stem cells is squirted over a matrix, stem cells may grow into a hunk of tissue that can later be transplanted into a waiting patient. Somehow, the matrix imparts critical organizing information to the cells.
Researchers have successfully created simple tissues such as skin, cartilage, and bone. More complex structures—an ear and teeth—have also been grown. But the hope is that a complex organ, like a ...