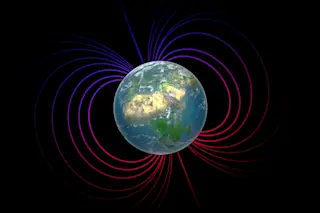
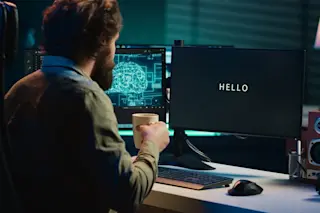
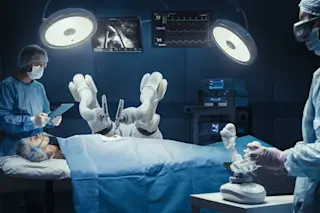
Dr. Charles Taylor would love to experiment with your arteries. He's a natural-born tinkerer, and the idea of operating on you only once and calling it a day seems less than ambitious to him. He's especially interested if you happen to be one of the millions of Americans who suffer from atherosclerosis: dangerous buildups of arterial plaque that hinder blood flow, causing pain, heart attacks, strokes, and in the worst case, death. Were you to hand over your clogged arteries to Taylor, he'd play vascular surgeon and gleefully perform as many as five, even 10 different surgeries on you. And before long he'd be wanting your heart, your liver, and your lungs in order to cut them, stitch them, and subject them to all sorts of pharmaceuticals. Ultimately, if his wish comes true, Taylor will have all your body— down to the last molecule— trapped right where he wants it: ...
Downloading Your Body
Operating in cyberspace will soon take the guesswork out of real-time surgery
More on Discover
Stay Curious
SubscribeTo The Magazine
Save up to 40% off the cover price when you subscribe to Discover magazine.
Subscribe