"I saved the most interesting case for last," said Molly Wilson, the resident who'd been on call the night before. It was a Saturday morning in early February. Molly and I had spent the last hour touring the Infants' Unit with the interns, stopping to discuss and examine each child who was unlucky enough to be inhabiting the unit that day. I was tired, the day was cold and gray outside, and I'd much rather have been at home in bed. But as the attending physician that month, the most senior doctor on the service, it was my job to make sure these children got the best care possible, and so fighting off the urge to daydream, I focused my attention on the resident. "This baby's name is Jarret Fox," Molly continued. "He's a three-month-old who was admitted last night for dehydration. According to his mother, Jarret stopped eating four days ago."
"Stopped eating?" I repeated, quickly coming to full attention. "What do you mean he stopped eating?"
"Just that," Molly replied. "His mom says that Jarret was happy and healthy a week ago. Then, on Tuesday, he seemed to lose interest in nursing. He just stopped sucking, his mother says, and he hasn't eaten anything since."
"That can't be right," I responded. "Three-month-olds don't just suddenly stop nursing and starve themselves until they get dehydrated."
"Well, I didn't believe it either at first, but the mother keeps telling the same story: she's been trying to force-feed him since Wednesday but hasn't had any success. Yesterday she brought him to her pediatrician. He said Jarret was about 5 percent dehydrated. He also said the kid was much floppier than he'd been the last time he'd seen him. So he sent him in for rehydration and a full evaluation."
That last part of Molly's report, the part about the increased floppiness, made my heart sink. It suggested a condition I hoped this baby didn't have. "Do you have any ideas about a diagnosis?" I asked.
"The only thing I can think of is spinal muscular atrophy," Molly said.
"That's what I'm thinking, too," I replied. "I hope we're wrong. Let's go see him."
Put simply, a diagnosis of the infantile form of SMA is a death sentence. A relatively rare inherited disease in which the nerves that control movement mysteriously degenerate and disappear, it is the childhood equivalent of the better-known (but no better understood) amyotrophic lateral sclerosis. As the nerves vanish during the first months of life, a child with SMA grows progressively weaker. After initial problems with feeding, the infant loses the ability to move its arms and legs. Breathing also becomes difficult. With time, the child becomes more and more hungry for air until finally, by about the first birthday, he or she dies. The cause is usually pneumonia, a common infection in lungs that aren't getting enough air.
As a medical geneticist, I have had the unenviable task of helplessly watching more than a dozen patients live out the nightmarish symptoms of SMA. The only thing I could do was aid families in coping with the loss of their children. As I entered Jarret Fox's hospital room that Saturday morning, the faces of all these children and their families flashed through my mind.
"Ms. Fox," Molly said as we approached Jarret's crib, "this is Dr. Marion. He's our attending pediatrician."
"Sorry we have to meet under these circumstances," I said with a smile as I shook her hand. Barefoot, clad in a peasant blouse and bell-bottom jeans, her long, straight hair parted down the middle, Jarret's mom looked like a long-lost refugee from the Summer of Love. She also looked as if she could use a good night's sleep. "How are you doing?"
"Not too well," she replied. "I'm hoping someone will be able to tell me what's wrong with my son."
"We're going to try to get to the bottom of it," I said. "First, maybe you can tell me the story from the beginning."
Without hesitation, Ms. Fox spilled out the short tale of her son's life. After an uncomplicated pregnancy, Jarret had been born at his parents' home in North Salem, a rural town north of New York City. He was the couple's second child: their daughter, Jessica, now three years old, was "healthy as a horse." Although his birth was attended only by a midwife, Jarret was examined on the first day of life by the family's pediatrician (the only one in the area who practiced homeopathic medicine and made house calls) and declared to be in excellent health. His mother could think of nothing unusual about her son's newborn period: in her words, he had been "like my other baby."
The infant had been seen by the pediatrician on a regular schedule, first at two weeks, then at a month, then at two months. He'd received his immunizations and had been growing and developing normally. Ms. Fox explained that her family were strict vegetarians who ate only whole, natural foods. She assured me that Jarret had had nothing but breast milk, adding proudly, "My daughter was exclusively breast-fed for the first 18 months of her life."
But four days ago this idyllic existence had ended. Jarret had simply refused to nurse. "He just wouldn't latch onto my breast," she said sadly. "Nothing I did got him interested. It was like a switch had been turned off in his brain and he wouldn't do it anymore. Just like that."
"Has he been hungry?" I asked, less certain now about the diagnosis.
"At first he was," she said. "That first day, he cried and cried. It was pathetic. But since then, he's just been lifeless, like he just doesn't care anymore."
I could see what Ms. Fox meant. Jarret was a sturdy, beautiful baby, but he lay as limp as a rag doll in his hospital crib, an IV in his left arm and a feeding tube in his left nostril. Although his eyes returned my gaze, Jarret seemed passive and expressionless.
"This doesn't sound like SMA," I said, shaking my head. After finishing my examination, I thanked Ms. Fox and told her that we needed to speak with the neurologist and that we'd be back later. Molly, a few interns, and I assembled in the corridor.
"SMA doesn't start suddenly like this," I began. "The weakness comes on gradually—the first day, the parents notice that the kid's a little floppy, the next day he's a bit more floppy, then a little more floppy the next, until finally they find they can't get him to eat enough to keep himself going. That's when the kid comes to the hospital with dehydration and the diagnosis is made. But this story of the weakness coming on suddenly like a switch going off—that's too acute to be SMA!"
"I agree," Molly said. "It sounds almost like the kid was poisoned."
+++
"Poisoned by what?" one of the interns asked. "The kid has had nothing but breast milk. If he was poisoned by something in the breast milk, the mother should have been affected, too."
"Good point," I replied, as a little bell of recognition began ringing in my head. "But Molly's right. It does sound as if he's been poisoned. And I think I know what it was." Without another word, I headed back into Jarret's room with the rest of the ward team trailing behind.
The mother, who had been sitting beside Jarret's hospital crib, rose to her feet.
"Sorry to bother you," I said. "But tell me again, when did you first notice this change in Jarret?"
"Tuesday afternoon," she replied. "When he woke up from his nap. He's usually starving when he wakes up. But that day, I couldn't get him to take my breast for anything."
I nodded. "And your three-year-old. Tell me, how does she get along with Jarret? Does she help you take care of him?"
"Oh, she's crazy about him," Ms. Fox replied with a smile. "She helps change his diapers, and when he spits up, she wipes him with a cloth. She tells me that I'm her mother, and she's really Jarret's mother."
I smiled at this also. "Since Jarret's exclusively breast-fed, she hasn't ever fed him, has she?"
"No, we'd never let her. But she always pretends to feed him. She pretends to spoon food into his mouth. It's really cute and they both love it."
"But as far as you know, she's never actually fed him?"
"Definitely not," Ms. Fox replied. "My husband and I are always at the table supervising. We'd never let Jess put anything in the baby's mouth."
I nodded and continued: "Ms. Fox, what does Jessica have for breakfast?"
The mother, somewhat surprised by the non sequitur, answered without hesitation: "A bowl of hot oatmeal and a glass of milk. Why do you ask?"
"Does Jessica eat the oatmeal plain, or does she put sugar on it?" I asked, already knowing what the answer would be.
As expected, Ms. Fox gave me an angry look. "Dr. Marion, we eat only whole, natural foods—no meat, no processed food, no sugar. Sugar is poison."
"Okay, no sugar," I pushed on. "But does Jessica use anything to sweeten her oatmeal?"
"We allow her to use a teaspoon or two of honey," she replied.
"Ms. Fox, we have to do some tests, but I think Jarret's going to be okay. I'm pretty sure he's got botulism."
It was Ms. Fox's reverence for natural foods that tipped me off to the possibility of infant botulism. That, and the suddenness of Jarret's symptoms. While considering the diagnosis as I'd questioned her, I visualized the scenario that had undoubtedly led to the baby's sudden onset of weakness.
Early that Tuesday morning, the Foxes were all in the kitchen. Jarret, sitting happily in his infant seat, had been placed at the table next to his sister, who was enjoying a bowl of oatmeal that had been topped with a few dollops of natural honey, straight from the hive. The children's parents had perhaps stepped away from the table to prepare their own breakfasts. Suddenly, Jessica, pretending to be Jarret's mother, silently offered her brother a spoonful of cereal. The infant eagerly accepted the offer and carefully rolled the strange-textured substance around in his mouth before swallowing. He smiled with satisfaction as Jessica, still in silence, finished off the bowl.
Later in the day, Jarret took his usual afternoon nap. When he awoke, his mother found that, mysteriously, he could no longer take her breast.
As Ms. Fox continued to answer my questions, I became more convinced that this scenario (or one like it) had occurred. It had to have: after hearing the story and seeing Jarret, there was no other logical explanation.
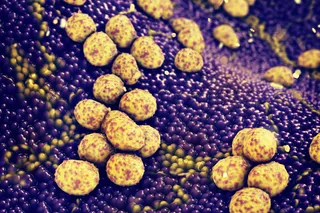
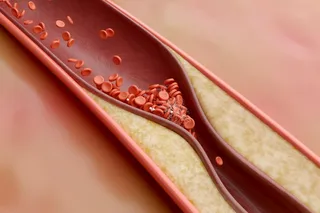
Like Ms. Fox, most Americans believe that when applied to foods, terms like "pure" and "natural" are synonymous with "healthy" and "nutritious." This may be accurate for most foods, but not honey. Eating honeyoin both natural and processed formocan lead to serious disease or even death in infants. Because of the environment in which it's produced, unprocessed honey often contains spores of Clostridium botulinum, the bacterium that causes botulism. The same can be true for processed honey. In most humans, the spores cause no problems: immune cells in the intestinal tracts of older children and adults release proteins that readily bind to and destroy the toxin. But in children under one year of age, infants whose intestinal tracts are still immature, the C. botulinum survives and starts making toxins. And that spells big trouble. After traveling through the gut's lining and entering the bloodstream, the toxins are carried throughout the body, where they bind to peripheral motor nerves, preventing them from carrying messages from the central nervous system to the muscles. Within hours of ingesting even tiny amounts of contaminated honey, previously healthy infants become profoundly floppy and lethargic, unable to smile or cry or suck. If the dose of toxins is large enough, every muscle, including those involved in breathing, becomes paralyzed. If their condition is not recognized quickly, these infants may simply stop breathing and die.
But if the diagnosis is made early, the prognosis for full recovery is good. Although there is no antidote to the toxin, its grip on the nervous system weakens with time. Gradually, the motor neurons create new receptors to replace those blocked by the toxin.
If the child is supported through this period—if he is tube-fed, provided with oxygen, and placed on a ventilator if breathing becomes difficult—he will eventually return to the state he was in prior to the disorder. The period of paralysis can last weeks or months.
When I told Ms. Fox that I believed Jarret had botulism, she looked at me as if I was crazy. But when the neurologist came by a few minutes later and agreed with the diagnosis, she began to have second thoughts about her initial impression. Later, when an emergency electromyogram (a test of Jarret's muscle and nerve function) revealed abnormal nerve responses consistent with botulism, she, too, became positively convinced of the story I'd invented.
Although we waited three long weeks for the lab reports, the results confirmed the presence of C. botulinum toxin not only in Jarret's serum and feces but in a specimen taken from the jar of honey from the Foxes' pantry as well. Because the scenario now seemed so obvious, I urged the Foxes not to confront or blame Jessica; doing so, I argued, would needlessly make the girl feel guilty. Rather, I suggested they have a talk with her, trying to get her to understand that she should never put anything into her little brother's mouth.
As for Jarret, it took him more than five weeks to return to his prepoisoned state, and his recovery was not without complication. On the afternoon of his admission to the hospital, his breathing had become labored, and when a blood-gas analysis revealed signs of respiratory failure, he was transferred to the icu, where he was intubated and placed on a ventilator. For weeks he remained dependent on machines, unable to breathe, suck or swallow, cry or smile, or move any of his muscles. He continued to be fed milk pumped from his mother's breast (she wouldn't allow him to be fed anything else) through the feeding tube.
Then in early March, his nurse noted what appeared to be a flicker of movement in his left leg. It was so subtle at first that she thought she'd only imagined it, but more movement occurred in the following hours. Slowly but surely, Jarret was regaining control of his nervous system.
In the next few days, he was gradually weaned off the ventilator. Soon the feeding tube was removed, and he began eating on his own again, first from a syringe, then from a bottle, and finally, more than a month after he had entered the hospital, directly from his mother's breast. Just about back to his old self, he was discharged in the middle of March.