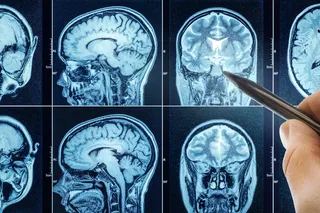
Imagine that this scientist kept a to-do list: On it would be a cure for cancer and, further down, understanding the diseases associated with aging. Elizabeth Blackburn is the 59-year-old Tasmanian-born scientist responsible for launching one of the hottest fields in the life sciences, the study of telomeres. These tiny strips of DNA cap the ends of chromosomes, and her research promises to yield potent therapeutics for many of the scourges that plague humanity.
The Cambridge-educated biochemist’s work has been honored with just about every major award in science—the Lasker, the Gruber, and the Gairdner prizes—and she recently made the list of Time magazine’s 100 most influential people. Telomeres drew her attention because of their crucial role in preventing the tips of chromosomes from fraying when a cell divides. Usually, when a cell makes a copy of itself, the telomeres shorten, which may explain why cells age and die. In ...