It is a dark night on a lonely highway outside Santa Fe, N.M. In the distance on either side of the road, you can still see the looming outlines of stately mesas.
“That’s all sedimentary rock up there. If you need to urinate, I’m happy to pull over,” Matt Lewin says as I glance out the window. “Some of the greatest fossil discoveries on Earth have been made from taking a piss.”
Lewin is not being sarcastic. For him, a drive down a New Mexico highway is something between taking a trip to Disneyland and being subjected to Chinese water torture. Miles upon miles of potential finds lie in wait, but each mile marker represents another lost opportunity. A few times he can’t contain himself, and we pull over to look at deposits by the highway.
“I’m not a snob,” he says at one point during the trip, examining an ordinary piece of petrified wood that most fossil hunters would probably ignore. “Something that lasted 35 million years or 100 million years, and it’s as beautiful as the day it was laid down.”

Lewin treats the victim of an accidental machete injury during a trip to Mount Banahaw in the Phillipines in 2011. (Credit: Darin Penneys)
Darin Penneys
Lewin is not a professional paleontologist. At best he is an enthusiastic amateur with an exceptionally good eye. Yet as an expert in “expedition medicine,” Lewin has been a part of some of the remotest digs on Earth. When a 1-ton dinosaur bone breaks a scientist’s leg three days’ travel from the nearest hospital, few people are better equipped to deal with it than him.
Lewin’s dual passions of medicine and fossils make for dizzying conversation as he switches, rapid fire, between how to fill a dinosaur footprint with plaster and how to use that same plaster to fashion an emergency cast. Back in the car, he lists famous fossil discoveries the way others recite baseball stats, and he holds forth on the many uses of safety pins in an emergency — like pinning an unconscious patient’s tongue to his cheek to prevent choking.
I am in New Mexico crashing Lewin’s vacation to learn how doctors working days away from civilization respond to emergencies with little more than intuition and a cooler full of medical equipment. Through a new institute he directs in San Francisco, Lewin has become the go-to guy for scientists worried about tropical diseases and exotic poisonous animals, by providing advice, logistics and referrals. But his pathway to expedition doctor was hardly direct.
A Career-Defining Moment
Matt Lewin was exposed to science as a small child by his father, an industrial chemist, and his aunt, who worked at New York’s American Museum of Natural History, where she would often bring her dinosaur-obsessed nephew.
But Lewin’s career-defining moment came when Carleton Gajdusek came to his second-grade classroom. Gajdusek had just won the 1976 Nobel Prize in medicine for unmasking a bizarre disease in Papua New Guinea called kuru, a byproduct of ritualistic cannibalism. His presentation was dazzling, with wild stories of jungle adventure. The laureate acted out stages of kuru, which often causes victims to shake or laugh spontaneously. The class was captivated, but none more than the little kid in the front row with the bright-red hair.
For Gajdusek’s grand finale, he brought out the brain and heart of a sheep. “When he dissected that heart, I was right there. And he opened it up and showed me the valves,” Lewin recalls. “I was the only person there. He was talking to me. That’s how I felt — all I remember is me and him.”
After that, Lewin decided to become an exotic adventurer, too. It was a career born of a childhood fantasy. He imagined himself an intrepid dinosaur hunter, trekking through deserts like the ones he saw pictured at the museums in search of the next Tyrannosaurus rex. Windblown, perhaps squinting to the horizon, he would brave scorching sun and exotic predators to save lives, just like Gajdusek did.

Lewin cares for a young patient during a maritime expedition to Indonesia in 2013. (Courtesy of Matt Lewin)
Matt Lewin
Classified ads for “desert adventurer doctor” are few and far between, so an aspiring student must build his own road map. Lewin got a degree in entomology from the University of California, Berkeley and started looking at medical schools. To avoid hundreds of thousands in debt, he enrolled in a University of Texas program that awards full scholarships to medical students who also complete a Ph.D. Afterward he chose emergency medicine — known for its short spurts of intense crisis — figuring this was as good a place as any to start.
In 2000 Lewin moved to New York for a high-octane ER residency in a part of the city where the emergency room was the closest thing many people had to health insurance. Here he was just one young physician among many, immersed in urban crises. The ER was less a place of Victorian-style contemplation and more one of constant turmoil and compromise, so Lewin struggled. He felt his dream of adventure and love of healing slowly slipping away.
Until one tragic day. It was cold and wet. After five consecutive shifts, Lewin was physically and emotionally exhausted. As he remembers, a woman in her 40s whom I’ll call Brenda (to protect her privacy) entered the emergency room, babbling incoherently, her body swollen beyond recognition. A flaky substance called uremic frost, likely the detritus of kidney failure, coated her skin, giving it a greasy feel. Lewin and the others realized she didn’t have much time. He told the husband and son to go to the waiting room as Brenda, paranoid and confused, screamed in the background.
“She was saying to her husband, ‘They’re going to kill me!’ ” Lewin recalls quietly, the memory vividly painted across his face. “She was crazy. She was insane with uremia, and yet she said this thing that was so … prescient.”
They needed to get an 8-inch catheter into her jugular vein to administer medication, but the attending physician, underequipped and overextended, said they didn’t have the resources to sedate her. He instead ordered another resident to hold down the hysterical Brenda so Lewin could insert a needle in preparation for threading the catheter. As Lewin lifted the needle, Brenda slipped out of the resident’s grip and vaulted onto the 3-inch spike in his hand, impaling her chest and puncturing her lung. She died minutes later.
The attending physician barely blinked as he moved on to the next crisis. Lewin, badly shaken, was left to inform Brenda’s son and husband that she had died, offering no other details. They quietly accepted the news, assuming she died as a result of her condition. “She would have died anyway,” Lewin remembers the attending physician saying.
From Low to High
After that, Lewin sank into a depression. He went home and wrote a list of the “Ten Things That Can Kill You Quickly.” The key for him was to separate the situations in which a doctor needs to rush from those that can benefit from him taking a step back. Choking, for example, or a potent toxin or cardiogenic shock, where the heart is too damaged to function — these things require fast action. In scenarios that didn’t make it onto his list, Lewin decided, physicians could take more time.
“Most diseases just don’t kill you that fast. It’s not like television,” he says. “If five seconds makes the difference, then probably the die is cast.” That was often the case in the emergency room, which was starting to feel more like a frenzied factory than a place for saving lives. He decided he had to pull away and focus instead on the list, which would later become his mantra.
10 Things That Can Kill You Quickly
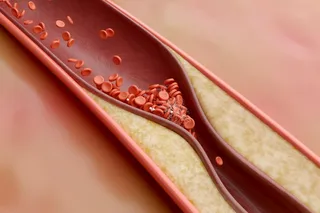
Cardiogenic shock: Heart cannot pump blood effectively for any reason, such as heart attacks. Some types of unusual heart rhythm also result in sudden death.
Neurogenic shock: A catastrophic drop in blood pressure due to damage to the nervous system. Stroke, bleeding into or around the brain and some broken-neck injuries fit into this category.
Sepsis: A whole-body inflammation in response to an infection. Often called “blood poisoning” by laypeople, it can happen in the lungs or skin and usually accompanies a fever. Left untreated, sepsis leads to multisystem organ failure.
Embolism: A blood clot or nitrogen bubble (the bends) that blocks circulation of blood from the heart to the lungs. Emboli can be pumped from the heart to the brain or other crucial organs, causing deadly complications.
Fluid and blood loss: Essentially, bleeding to death or severe dehydration. When large amounts of fluid leave the body, blood pressure falls dramatically.
Toxic-metabolic-environmental problems: Lewin lumps venoms, poisons, acute electrolyte, glucose and hormone disturbances into one category relating to body chemistry and extreme exposures.
Tension pneumothorax: A hole in the lung that creates a one-way air valve. Air traps in the chest and eventually compresses the heart. It can, potentially, be relieved using a large needle.
Tamponade: An accumulation of fluid or blood around the heart that compresses the heart and causes dangerous drops in blood pressure.
Anaphylaxis and similar reactions: An extreme allergic reaction that can, with fast action, be reversed with drugs like epinephrine.
Choking: This danger can arise from swallowing an object, but also from swelling or trauma. “Everyone should be educated in handling this fatal emergency in babies and adults,” Lewin says.
Lewin began spending more time at the Natural History Museum, hanging around the fossils. He needed a change, but as he withdrew emotionally, his performance reports tanked, and he was no longer an attractive transfer to the other hospitals where he applied. But one spring day in 2001, an email popped up on his screen. It read, “Matt, Herb Bivins here. You don’t like New York. Call me.”

Lewin explains to researchers how to use an injectable snakebite antidote — a conversation that inspired him to make a nasal spray as an alternative. (Credit: Natalia Chousou-Polydouri)
Natalia Chousou-Polydouri
Bivins was head of the University of California, San Francisco’s emergency medicine program in the Central Valley town of Fresno. The program is legendary in the field of wilderness medicine, which refers to the practice of medicine with minimal equipment in remote places. The program is housed in the only major trauma center near the Sierra Nevada, so its doctors handle serious wilderness injuries, such as lightning strikes and snakebites, up and down the mountain range. They also train and advise backcountry medics in several national parks as far away as the Grand Canyon. Their research is a broad mix that includes the long-term effects of rattlesnake venom and new ways to reduce a dislocated hip.
Bivins had gotten Lewin’s inquiry and decided to take a chance. At the same time, Lewin overheard a conversation in the museum about two paleontology students who became sick in Mongolia. They got better, but the team was nervous about the mysterious disease. Lewin bolted home to read everything he could on Mongolian diseases and wrote the expedition leader — famed paleontologist Mark Norell — begging for a chance to figure out the diagnosis. Norell took a shine to the eager doctor and agreed. So Lewin asked for blood samples from other paleontologists who visited the region; being scientists themselves, they were happy to roll up their sleeves. Four other members of the expedition had gotten sick, and all of them showed antibodies for North Asian tick typhus, although only two remembered being bitten. Lewin sketched out a paper on the tick-borne infection (later published in The Lancet) and packed his bags for Fresno.
An Accidental Discovery With roots as an agricultural town out of The Grapes of Wrath, Fresno has gangs, high poverty rates and a downtown that is frequently voted the worst in the state. But Lewin thrived there. Fresno offered what New York couldn’t: a different way to look at medicine. In the Fresno ER, he treated the usual gunshot wounds and drug overdoses, but he also got to see hikers and climbers, teach medicine to backcountry rangers and give lectures on venomous insects.
Then in 2003, he got a call from Norell. Asia was gripped in panic over the viral respiratory infection SARS, and Norell was nervous about his upcoming dig in Mongolia’s Gobi Desert. Remembering the quirky redheaded doctor’s eagerness to treat his former crew, Norell invited Lewin to accompany the Mongolian expedition as a medic and fossil spotter.
Most of Lewin’s medical work turned out to be keeping people hydrated and upright. (Cracked and blistered feet are a common problem in the Gobi.) He patched up feet, treated sunburn and worked his turns in the kitchen. Then one day, on the way back from a dig, he spotted an odd spherical rock half-exposed in the sand. Looking closer, he discovered it was a dinosaur egg.
A dinosaur egg is rare, but even more so if the embryo is still inside. The only way to confirm it would be to X-ray the egg. So he cataloged it, carefully packed it in a medicine bottle, and flew it to San Francisco. At 3 a.m. he went to the CT scan lab at Fresno’s parent campus in San Francisco, registered the fossil as a patient named Egg Kernberg, and scanned it. Inside were forelimbs, legs, scattered vertebrae, the mandible and the base of a skull, all from a distant relative of Triceratops. Eventually, Lewin’s discovery found its way onto the cover of the prestigious German journal Naturwissenschaft.
After that, Lewin was a fixture on Gobi fossil trips. He took a job teaching at UCSF and working in its emergency room. The academic calendar allowed him to duck out every year for Mongolia or any of half a dozen other countries. The more trips he went on, the better a medic he became and the more eclectic his publishing. Over the next few years, he co-published papers on performing emergency throat incisions with a hollow plastic spike; the discovery of a large, birdlike dinosaur; the defensive behavior of moth larvae; and how to hum to make your jugular vein more accessible.
Dan Bishop/Discover
Meanwhile, he patched up a Mongolian porter who tripped over an open manhole and saved another’s life after a cut led to an infection that got out of hand deep in the Gobi. But it was not just cuts and antibiotics. Long, lonely hours in an unfamiliar place can drive some people to drink heavily, get in fights or become depressed. Others just make really bad choices. On one of his earliest expeditions, Lewin brought an acidic callus-removal cream that rapidly dissolves layers of skin. Despite a large, handwritten label reading “Not for face, lips or masturbation,” a male student had quietly raided his med kit, leaving Lewin to treat the badly placed wound.
On that same trip, Lewin saw that some doses of Vicodin, an addictive painkiller, had gone missing. Trusting his team members, he hadn’t thought to keep the narcotic under lock. Then he noticed some members of his crew acting “unusually chipper.” Lewin confronted one of the students, who denied stealing the drugs until Lewin pointed out that with pupils the size of pinpoints, the student was clearly high.
Guerilla Tactics
The oddest use of Lewin’s skills came in 2005. During another project in Asia, a group of armed men claiming to be local park enforcement descended on the camp and halted the dig. They asked the team to contribute to a “wilderness restoration fund.”
This obvious demand for a bribe rankled the government minder assigned to watch the team. The minder was from a higher social class than the armed men and refused to pay, calling them “primitive sheeplike people.”
With some members of the crew now afraid for their safety, Lewin found himself on hazardous moral ground. A patient who puts his life or the life of others in danger loses the right to make his own decisions and can be restrained or sedated. So after conferring with the team leader, he offered a glass of wine containing a sedative to the minder, who had been drinking heavily already. He passed out shortly after, allowing the team to pay and make apologies to the bandits, who soon left in peace.
When not on expeditions, back home outside San Francisco, Lewin treated all manner of exotic parasites in scientists returning from the field. In 2004, a scientist who had been surveying elephant seals in Greenland turned up with seal finger — a swollen, purple, bacteria-induced blister found in seal hunters. Then there was the researcher, just back from Myanmar, panicked about a tumor in his lung. Lewin knew that some rare Asian worms form benign cysts in the lung, so he suggested the man get a biopsy before planning an operation. The biopsy came back clean.
Exotic adventures do not pay the bills, so Lewin continued to work in San Francisco ERs. But his guerrilla tactics were not always appreciated in the big city. It wasn’t just the crazy hair or regular use of tuxedo T-shirts that riled some colleagues. It was his willingness to abandon standard procedures for what he perceived to be a better solution. When a woman without insurance came to him with a nasty laceration to the head, Lewin sealed the wound by tying the long strands of hair on either side of it together, like laces on a shoe, so the patient could avoid paying to remove stitches. Although this is technically an acceptable treatment, his boss asked him to leave the “Gobi tactics” in the desert.
Bitten
Not exactly at home in big-city ERs, Lewin decided in 2008 to take a unique position as a medical adviser to the California Academy of Sciences in the heart of San Francisco’s Golden Gate Park. The academy is famous for its bright, sunny museum filled with wonders from around the world. Behind the scenes is a maze of offices and storage units carrying bugs, birds, lizards and slimy, furry, stinging critters from every continent on the globe.
People there are welcoming and enthusiastic — a byproduct of working at a museum. But there is one topic no one will discuss. In 2001 Joe Slowinski — a much-beloved, cheerful Midwesterner — was one of herpetology’s rising stars, wrangling the world’s most dangerous snakes with superhuman ease. That September, he took an academy expedition to the farthest reaches of the Burmese jungle, cataloging new species of reptiles and amphibians. Reaching into the wrong collection bag one morning, he pulled his hand out with a banded krait — one of the world’s most lethal snakes — attached. The venom quickly blocked communication between Slowinski’s neurons and the muscles they controlled, causing progressive paralysis that made his diaphragm limp, preventing him from breathing. His lungs stopped working, and a little over a day later, he died.
Seven years later, Lewin became a go-to guy for scientists preparing to go into the field. He put together first-aid kits, advised safety measures and planned for emergencies. He helped retool the academy’s safety standards, running drills to test and fine-tune protocols for responding to emergencies such as venomous fish bites. He helped design a new system of checks, complete with color-coded labels, to safeguard his colleagues in real life. And in 2010, he created the Center for Exploration and Travel Health, a clearinghouse that academy scientists working in remote sites can turn to for referrals to expedition doctors; it even includes Lewin’s home number — which they can call at all hours — in case disaster strikes.
With the center now running, Lewin has turned his attention back to Slowinski and what he calls “the biggest gap in field treatments for 10 things that can kill you quickly.” Namely, snakebites.
Snakebites kill nearly 100,000 people worldwide each year, mostly in the developing world. Those who get to a hospital in time receive antivenom and are put on life support, which keeps them breathing until the venom clears their system. But in the field, the only effective treatment is to give a patient mouth-to-mouth for hours or even days. What bite victims in the wilderness need most, therefore, is time. And Lewin thinks he has found a solution. Two common drugs — neostigmine and glycopyrrolate — could buy a victim some time. As the venom snips the lines of communication between the neurons and muscle, the drugs work to enhance the signal — like sending a surge of electricity down an increasingly fraying wire.
Lewin has come up with a travel-friendly nasal spray incorporating the two drugs that could be used in dozens of snake-riddled countries. Last year, after tinkering with the doses on himself, he tested the treatment in the lab. Sure enough, it worked. Now he is searching for funding to build a pilot project to put the spray through clinical trials and eventually distribute a refined product in countries like India, where snakebites cause thousands of deaths before victims can reach the hospital.
Could this nasal spray have saved Slowinski? Maybe. Rais Vohra, a Fresno colleague who advised Lewin in the early stages of his research into the antidote combination, says, “This is not going to be a definitive treatment. It may not do much but buy a few hours. But that much might count.”
The Killer List Revisited
Today Lewin has forged the alternate path he first imagined a decade ago while sitting among museum fossils, lamenting the death of a woman from an ER procedure gone wrong. He still works part time in ERs, and when he sees patients, he runs through his list of killers (updated these days with all manner of clauses and addenda). If the problem is not on the list, he takes a step back. The litany “is my daily prayer. It’s my calisthenics,” he says.
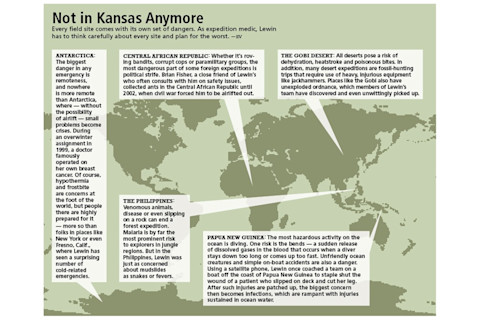
Whether in the ER or the Gobi, the list of quick killers dictates how Lewin thinks about treatment and evacuation. Expeditionary medicine is about good decisions coupled with preparation. Over the next year, he’ll fly to Papua New Guinea, India, Australia and Argentina. Before his plane touches down in each, he will be able to recite all the local diseases, venomous snakes, frogs, bugs, and fish, and poisonous plants. He will know where the medical facilities are, what equipment they have and what’s broken. He also keeps a list of classically Lewin-esque research questions to explore: How well does honey treat wounds? Can raw eggs make a suitable field dressing? Does hot water actually release a Gila monster’s jaws?
We’ve reached the end of our New Mexico road trip, and we have scoured the side of the road for long-dead sea creatures, found a shark tooth in an ancient seafloor and tracked long-dead worms across fossilized mud. Today, Lewin has managed to pull a few strings to get us a backstage look at the legendary Ghost Ranch. In addition to being the stunning backdrop for countless movies, for 125 years this sandstone formation has yielded a continuous line of important Triassic dinosaurs, like Coelophysis and Dromomeron.
Kneeling next to an active dig of an ancient crocodilian creature, Lewin admits that he is not a paleontologist, but he can pore over a find like this for hours. This quality may seem incongruous with the adrenaline-infused ER, but Lewin disagrees and points to the fossil. “It has a story. Same thing as when you are seeing patients. You are trying to figure out the story,” he says. The story of a 200-million-year-old animal or a single disease — the only difference is the pace.
[This article originally appeared in print as "On Call in the Wild."]
Matt’s Must-Have Med Kit
It’s impossible to prepare for every emergency, but in addition to standard first-aid supplies, there are a few things Lewin rarely leaves civilization without.
Safety pins: Lewin prefers medium or large. They’re crucial for turning shirts into slings, and they can be heat-sterilized and used to relieve blood trapped under a toenail.
Heavy-duty nail clippers: Crucial to a happy team are happy hands and feet. Hangnails, ingrown toenails and other slight discomforts for city dwellers can be misery in the backcountry.
Skin stapler and staple remover: Lewin is a huge fan of these. Like a normal stapler (but not to be swapped with one), skin staplers punch stainless-steel clips over a wound to close it.
Sugar: Never assume that a diabetic has brought it. Lewin brings granular sugar, which he also uses to clean wounds.
Baby aspirin: This is less for pain and more for heart attacks and strokes, which demand a fast blood thinner. The small-size pills allow Lewin to administer just the right dose.
Thermometer: Amazingly, many people don’t think to pack this medicine-cabinet staple into their roving med kits. But if a patient has a fever, this is a crucial tool. Taking regular temperature readings will help you distinguish minor bugs from life-threatening disease.
Fingertip pulse oximeter: Combined with a thermometer, a finger oxygen sensor — available at many drugstores — gives a great read on vitals. It distinguishes between someone who is in real trouble and someone who is just short of breath.
Presence of mind: If you have nothing else, this is the most important asset you can bring into the wilderness.