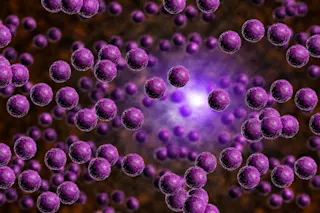
Ninety years after the discovery of the first antibiotic, penicillin, researchers have found an entirely new tactic in the fight against bacteria that cause infectious diseases. Instead of hunting for new ways to kill bacteria, researchers have developed a drug, called LED209, that disarms them, preventing them from releasing the toxins that cause illness.
"The sensors in bacteria are waiting for the right signal to initiate the expression of virulent genes," [said lead researcher] Vanessa Sperandio.... "Using LED209, we blocked those sensing mechanisms and basically tricked the bacteria to not recognize that they were within the host" [Reuters].
The new technique, which has only been demonstrated in mice so far, could be a boon for researchers who are worried about creating more antibiotic-resistant "superbugs." Superbugs evolve when a few bacteria mutate into a form that can survive a dose of antibiotics; those few that survive are given a huge boost ...