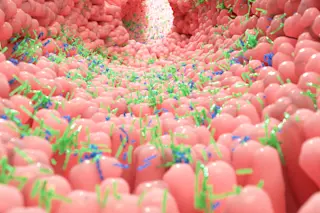
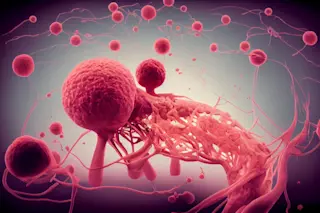
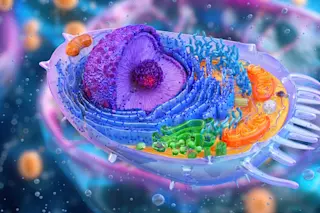
By now most people are familiar with philosopher Daniel Dennett’s characterization of natural selection as Darwin’s dangerous idea-- dangerous because it acted as a corrosive acid capable of dissolving the established structures of human society. That acid can be just as corrosive of scientific structures, which one might have thought more impervious to the damage. Thus a Darwinian idea has eaten away at some of the foundations of my own field of research for the past half-century, tumor biology, and forced cancer researchers to reexamine some cherished notions about the origins of cancer that were current during the first half of the century. Today, with the discovery of new genes that contribute to the development of cancerous cells, we are keenly aware that cancer is, above all, a disease of DNA. But more important, we know that this disease does not occur in a preprogrammed manner. Only through the gradual ...
Malign Evolution
In 1911 a hen's tumor prompted a 70-year search for cancer-causing viruses. What it ultimately revealed were the rules of a Darwinian game, played to the death.
More on Discover
Stay Curious
SubscribeTo The Magazine
Save up to 40% off the cover price when you subscribe to Discover magazine.
Subscribe