Mommy, where do babies come from? Parents have dreaded this question ever since the stork made its first delivery. But today’s mommies and daddies have more explaining to do than their own parents could possibly have imagined. Though the birds and bees discussion was never easy, its elements were fairly straightforward: the fireworks exploding, the train chugging through the tunnel, the waves pounding the shore, the occasional reference to anatomy. Once upon a time, baby-making was synonymous with whoopee-making, and frozen eggs were for pastry dough, and seven was how many times you should let the phone ring before you hang up, not how many fetuses you could fit in a womb.
These days, though, the facts of life can sound a lot like science fiction, as late-twentieth-century humanity grapples with the rise of noncoital conception. There are now more than a dozen ways to make a baby, the vast majority of which bypass the antiquated act of sexual congress. The last three decades have seen the advent of such high-tech interventions as fertility drugs, in vitro fertilization, donor eggs, donor sperm, donor embryos, and surrogate mothering. In the works are still more advanced technologies, such as the transfer of cell nuclei, embryo splitting, and even, if at least one man has his way, the cloning of human adults.
These techniques generally are gathered under the heading of assisted reproduction. All the ones in use today were pioneered for and are usually employed by infertile couples of childbearing age. But they are also used by people with less conventional notions of parenting—singles, postmenopausal women, and gay partners. In the near future, assisted reproduction may become standard procedure for anyone who wants to conceive, and who can afford it. The allure, of course, is control: control over the timing of parenthood, control over embryo quality, control over genetic disease, control over less pernicious characteristics, such as gender, that are also determined by genes.
So far, owing to federal policy and societal preference, the practice of assisted reproduction is largely unregulated. One specialist has even called it the Wild West of medicine. It’s also expensive, bothersome, inefficient, and fraught with ethical complications—but none of those considerations has slowed its growth. Since 1978, when the first test-tube baby was born, the number of fertility clinics in the United States has gone from less than 30 to more than 300. The multibillion-dollar fertility industry has created tens of thousands of babies. Assisted reproduction has relieved the anguish of men and women who, just decades ago, would have had to abandon their hopes of having children. It’s also created a world where a dead man can impregnate a stranger, where a woman can rent out her uterus, and where a child can have five parents—and still end up an orphan. It’s not at all clear how this new world will change the meaning of family. But it has already transformed what used to be known as the miracle of birth.
Last November in Iowa a couple in made history, national television, and the covers of Time and Newsweek when their seven babies were born alive. We’re trusting in God, the McCaugheys told reporters when asked how they would cope with the sudden surfeit of offspring. But to conceive for the second time, Bobbi McCaughey had trusted in Metrodin, a fertility drug that stimulates the ripening of eggs in the ovaries. A woman on Metrodin can produce dozens of eggs in a month instead of just one.
Metrodin belongs to a suite of hormones that are used to increase egg development and release, or ovulation. Fertility drugs go by many brand names, like Clomid, Pergonal, Humegon, Fertinex, Follistim, and some have been around for decades. Women who have problems ovulating regularly can often conceive by the time-honored method once fertility drugs have improved their chances of success.
Even so, taking fertility drugs is not like taking aspirin. Most are administered by daily injections that couples are trained to perform. The drugs themselves aren’t cheap—a single dose of Fertinex, for example, is about $60—and most doctors monitor the progress of egg ripening with ultrasound scans and blood tests that add to the overall cost. Ultimately, a cycle of treatment with fertility drugs may cost more than $1,500.
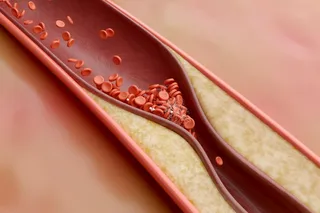
And there are risks. The most common is multiple pregnancy: the simultaneous conception of two or (many) more fetuses, like the McCaugheys’. Despite the celebratory atmosphere that greeted the Iowa septuplets, such pregnancies are in fact a grave predicament for would-be parents. Multiple pregnancies increase the odds of maternal complications such as high blood pressure and diabetes. And they pose even greater risks for the unborn. The fetuses gestating in a multiple pregnancy are far more susceptible than their singlet peers to miscarriage, birth defects, low birth weight, and premature birth, as well as lifelong problems that can result from prematurity—including cerebral palsy, blindness, kidney failure, and mental retardation.
There are ways to get around the problem of multiple pregnancy. One is to abstain from sex if ultrasound scans reveal that a plethora of eggs is poised for release. Statistics suggest, however, that many couples choose not to exercise this option. Whereas in the general population the rate of multiple pregnancy is 1 to 2 percent, the rate among women treated with fertility drugs can be as high as 25 percent.
Another way to deal with the risks of multiple pregnancy is to eliminate some fetuses before they are born. Infertility specialists call this technique selective reduction. It is performed before the third month of pregnancy by injecting selected fetuses with potassium chloride, which stops the heart. A doctor inserts a needle through the abdomen or vagina of the mother-to-be to deliver the injection.
Like most techniques of assisted reproduction, selective reduction introduces ethical problems as it solves medical ones. For many couples, the decision of whether and how much to reduce is traumatic. Some, including the McCaugheys, simply refuse to do it. Others accept the agony—and irony—of destroying surplus fetuses as an unfortunate consequence of their condition. Yet still other people feel comfortable enough with the technique to use it for practical, rather than medical, reasons. There are patients that will push very hard to reduce from three fetuses to two, says Benjamin Younger, executive director of the American Society for Reproductive Medicine. They’ll say, ‘Doctor, I can’t cope with triplets.’
If an infertile couple chooses to pursue the more advanced procedures of assisted reproduction, selective reduction is only one of several trials they may face. I don’t think I’ve ever done anything as difficult, admits a Boston woman who became pregnant after two years of ever-escalating interventions. You have to really want it.
Kathryn Graven and her husband decided to start a family when Graven was 34. After nine months of trying by the usual route, they went to an area clinic for a fertility workup. There are various causes of infertility, including hormonal imbalance in women, low sperm count in men, and blockages in the reproductive tract of either partner. But tests failed to identify a specific cause for the Gravens’, so their doctor recommended conservative treatment. In each of three months, Graven tried the fertility drug Clomid, which is taken orally, to stimulate egg production, followed by artificial insemination with her husband’s sperm. When that didn’t work, Graven switched to Fertinex, which is injected beneath the skin. After two rounds of Fertinex and artificial insemination also failed, the couple decided to try in vitro fertilization.
IVF is the cornerstone of assisted reproductive technology. The procedure—in which ripe eggs are removed from the ovaries and incubated with sperm—greatly improves the haphazard gambit of traditional in vivo fertilization. It also introduces another level of complexity and expense. In addition to egg-ripening hormones, a woman undergoing IVF will usually take a protean cocktail of drugs designed to suppress and then trigger the release of mature eggs. Egg retrieval, done by guiding a hollow needle through the wall of the vagina and into the nearby ovaries, is characterized as a minor surgical procedure. (The next day I felt like a Roto-Rooter had gone through my insides, says Graven.) And then the fertilized embryos have to be transferred back to the uterus.
When Graven’s IVF attempt failed as well, her doctor recommended a more advanced technique: gamete intrafallopian transfer, or gift. In this procedure, eggs are harvested, mixed with sperm, then returned to the fallopian tubes—where egg and sperm normally meet—to fertilize. gift requires a longer and more complicated operation, with three incisions in the patient’s abdomen, and about two days’ recovery. But the success rates are 5 to 10 percent higher than those of ivf. It worked for Graven: she is due to give birth in July, at the age of 37.
GIFT is one of several variations on the IVF theme that were introduced in the 1980s as infertility specialists sought to expand their skills in assisted reproduction (see sidebar, page 80). Even with these innovations, however, the efficacy of assisted reproduction is sobering. Graven’s experience was typical of what many infertile couples might undergo, except in one respect: Graven got pregnant. Success rates for ivf depend on a patient’s age and vary from clinic to clinic and from procedure to procedure. But the ballpark figure—the so-called take-home baby rate—is one live birth for every five ivf cycles. Infertility specialists point out that the success rates for these procedures increase every year and that in any given month a fertile couple’s chance of conceiving by traditional means is also one in five. According to the American Society for Reproductive Medicine, more than half of all infertile couples could attain pregnancy if they persisted long enough with treatments for assisted reproduction.
But that also means that about half will never have a baby, no matter how much therapy they get. And one thing about making babies by the usual means is that it’s free. If at first you don’t succeed, you can try, try again, without taking out a second mortgage. A single cycle of ivf, on the other hand, costs between $8,000 and $10,000. Special options like gift may cost more. Graven didn’t have to pay for most of her treatment, because Massachusetts is one of ten states that mandate insurance coverage for infertility treatment. The bill for her pregnancy would have been well over $25,000.
Is it worth it? The market says yes. Although rates of infertility have remained constant, demand for infertility services has risen steadily in the past two decades. Today about 6 million couples in the United States have fertility problems; half of them go to their doctors for help, and about a quarter end up trying assisted reproduction. Whether those couples view these attempts as a blessing or a curse depends on the outcome, says Margaret Hollister, director of the help line at resolve, a national infertility support group based in Somerville, Massachusetts. The treatments are stressful, expensive, and require a big time commitment.
Of course, the same could be said of parenting. The stress associated with infertility, however, may be especially pernicious. Alice Domar, director of the behavioral-medicine program for infertility at Beth Israel Deaconness Medical Center in Boston, has found that women who have been trying to get pregnant via assisted reproduction for two years or more have rates of depression as high as those of patients with cancer, heart disease, and aids. She also finds that conception rates in severely depressed patients improve when the depression is treated.
Domar has used her results to argue that infertility should be regarded as a serious medical condition and that more research needs to be done on the connection between mind and reproductive machinery. Trouble is, Domar’s studies don’t ascertain whether her subjects’ depression is caused by the trials of infertility per se or by the tribulations of infertility treatments. Infertility patients describing their encounters with assisted reproduction use words like roller-coaster ride, addiction, and obsession. Fertility drugs are renowned for causing moodiness, as well as cramping, weight gain, and bloating. And the demands of tracking ovulation can turn a person’s world upside down. During some parts of the cycle, a patient might visit her ivf clinic once or even twice a day for blood tests, ultrasound scans, and injections. Your life starts revolving around the beginning, middle, and end of your cycle, says Graven. Monitoring your body becomes a full-time job.
Moreover, pursuing parenthood via assisted reproduction means being confronted with ethical decisions well outside the range of most people’s moral radars. Because ivf techniques often give rise to multiple pregnancies, selective reduction is an issue here as well. Couples undergoing ivf must also decide how many eggs to fertilize and transfer at one time (which bears on the question of multiple pregnancy), whether they want to create and freeze embryos for future use, and what the eventual disposition of any unused frozen embryos should be. Former spouses have waged custody battles over frozen embryos, and in at least one case the attending ivf clinic claimed the embryo as its lawful property. Legally, human embryos occupy a gray area all their own, somewhere between human life and some rarefied form of property.
Assisted reproduction also invites the preselection of embryos based on genetic traits, and all the moral dilemmas that may accrue thereto. Screening is done by removing a single cell from an eight-cell embryo and analyzing the chromosomes or dna in the cell nucleus. Already some clinics offer to screen in vitro embryos for genes related to cystic fibrosis, hemophilia, and muscular dystrophy. Couples can decide which of the embryos they’ve created meet their specifications; the rejected embryos can be discarded or donated to research.
Finally, assisted reproduction has opened the door to all manner of gamete swapping and surrogacy, from the simplest and oldest method—artificial insemination with a donor’s sperm—to more complex scenarios in which any combination of donor eggs, donor sperm, and donor embryos may be used. In addition to biological surrogate motherhood (the method that created the celebrated Baby M), gestational surrogates will agree to carry and give birth to a baby to whom they bear no genetic relation whatsoever. It is now possible for a person to have a baby by procuring eggs and sperm from donors and hiring a birth mother to do the rest (this has been done). It is possible for a woman to use a birth mother for cosmetic reasons or convenience alone (this has also been done). It is possible for the sperm of dead men to be retrieved and used to impregnate their widows (likewise). It is possible for women long past the age of menopause to give birth (this, too, has already happened).
Another exceptional birth captured headlines last October, when a woman whose ovaries were nonfunctional delivered two healthy boys courtesy of Reproductive Biology Associates in Atlanta. rba had engineered the twins’ conception using donor eggs frozen for more than two years. Because the sheer size and complexity of the human egg make it more susceptible than sperm to damage during freezing, protocols for the cryopreservation of eggs have been difficult to perfect. Until recently, in fact, most attempts at egg freezing have failed. The twins are the first of their kind to be born in the United States.
Though RBA’s achievement was quickly overshadowed by the arrival of the Iowa septuplets, the egg-freezing feat has more significant ramifications. Once it becomes widely available, cryopreservation will offer a unique opportunity to women: the chance to store their young eggs for use at a later date. Defects in aging eggs are thought to be responsible for the declining fertility of older women; indeed, donor-egg technology has demonstrated that the rest of the female reproductive apparatus withstands the test of time. By assuring women a lifetime of viable gametes, egg freezing could let them beat the biological clock.
Of course, women would then be using assisted reproduction for their own convenience rather than for treatment of an existing medical condition. In this respect, egg freezing echoes a common theme in assisted reproduction. Current techniques were developed to help patients with specific medical problems—egg freezing, for example, will allow cancer patients whose eggs would be destroyed by radiation to set aside some gametes prior to therapy. Yet inevitably, the fruits of infertility research expand reproductive options for all men and women. And these choices are not always easy to live with, for individuals or for society.
A striking example comes from the laboratory of reproductive endocrinologist Jamie Grifo at New York University Medical Center. In another effort to beat the biological clock, Grifo is transferring the nuclei from older women’s eggs into younger eggs from which the nuclei have been removed—that is, enucleated eggs. When these hybrid cells are artificially stimulated to divide, the transferred nuclei don’t show the chromosomal abnormalities typical of vintage eggs. Grifo’s work is still in the research stage, but he hopes eventually to fertilize such eggs and implant them in his patients.
Grifo is not cloning humans, but his experiments draw on established mammalian cloning technology. Lamb 6LL3, better known as Dolly, was created by nuclear transfer from an adult cell to an enucleated egg. Grifo emphasizes that he’s concerned only with transfers between egg cells for the purpose of treating infertility; he says he is strongly opposed to human cloning, and that in any case it will take years for researchers to figure out how to do it. But the fact is, it’s possible, he says. I just can’t think of any clinical indications for it.
If Grifo can’t, someone else can. Richard Seed, a physicist turned infertility entrepreneur, made headlines in January when he announced that he was seeking funds to establish a laboratory for the cloning of adult human beings.
The National Bioethics Advisory Commission recommended a ban on human cloning back when Dolly first saw daylight. More recently, President Clinton reiterated his call for a five-year moratorium on human cloning research. But the American Society for Reproductive Medicine, which issues ethical guidelines for the use of assisted-reproduction technologies, has taken the middle ground. We do not support the cloning of an existing—or previously existing—individual, says Younger. But that is not to say that cloning technology is bad. Cultures of cloned nerve cells, for example, could be used to treat spinal-cord injuries, he says. We would not like to see research curtailed.
The society has also come out in favor of continuing research on embryo twinning—a procedure, done so far only in animals, in which a single embryo is divided to create two genetically identical individuals. The society’s rationale is that the technique of embryo twinning could provide infertile couples with twice as many embryos to implant. But the distinction between cloning and twinning grows obscure if, say, one of the twinned embryos is frozen until its sibling has grown to adulthood.
Critics of assisted reproduction fear that today’s innovations will become tomorrow’s imperatives. Already some infertile couples feel entrapped by the catalog of choices. All these technologies, by providing more and more options, make it very difficult to say, ‘No, we’ve tried enough,’ says R. Alta Charo, a law professor at the University of Wisconsin and member of the National Bioethics Advisory Commission. Choice is not a bad thing—but neither is it an unalloyed good.
And lack of regulation only exacerbates the problems surrounding assisted reproduction. This field is screaming for regulation, oversight, and control, says Arthur Caplan, a noted bioethicist at the University of Pennsylvania. What keeps us from doing so is the notion that individuals should have procreative freedom.
Rancor over abortion has also impeded the regulation of technologies for assisted reproduction. Since the 1970s, the United States has outlawed federal funding of research on human embryos or fetal tissue in response to concerns that such research would encourage trafficking in embryos and fetuses. The ban has not been applied to privately funded efforts, however; consequently, most research on assisted reproduction has been conducted beyond the reach of federal regulation and oversight.
Specialists in assisted reproduction, including Grifo, say this is just as well—that regulators wouldn’t appreciate the technical and moral complexities of the work. But with the bulk of experimentation going on in private clinics, patients—and their children—can become guinea pigs. Even when couples are not directly involved in experimental procedures, they may be confronted with uncomfortable choices, such as financial incentives to donate their gametes or embryos.
People often feel compelled by the circumstances—‘What else could we do?’ says Barbara Katz Rothman, professor of sociology at Baruch College. I’m not sure how we should make these decisions, but I’m pretty sure they shouldn’t be made by the market.
And market forces affect more than just infertile couples. Although eggs are far more scarce and difficult to obtain than sperm, young women donors are typically given minimal compensation for their time and trouble. But in February the New York Times reported that St. Barnabas Medical Center, a fertility clinic in Livingston, New Jersey, has begun offering young women $5,000 to donate eggs—a price reported to be twice that of competitors. Unlike payment for organs, which is illegal, limited payment for eggs is legal. The professional guidelines of the American Society for Reproductive Medicine deem them body products, not body parts.
Many observers fear that it is not the participants in assisted reproduction but their children who may suffer most from the imprudent use of these new technologies. For example, with the rising popularity of assisted reproduction, more and more children are being exposed to the risks of premature birth: since 1971 the annual number of multiple births in the United States has more than quadrupled. Scientists and ethicists alike have spoken out against helping single, postmenopausal mothers conceive, arguing that it is morally reprehensible to create children who may well be orphaned. Some question the wisdom of arrangements—like surrogacy or gamete donation—that could diffuse the responsibility of parenthood. And some researchers are concerned with the safety of the procedures themselves for assisted reproduction. A recent—and controversial—Australian study of 420 children suggests that babies produced with the aid of intracytoplasmic sperm injection, in which a single sperm is injected into an incubating egg cell, are twice as likely to suffer major birth defects of the heart, genitals, and digestive tract.
Everything we do in vitro to a mammalian embryo causes it stress, says Robert Edwards, the specialist who presided over the first test-tube baby 20 years ago. But there’s immense responsibility in the scientific community to evaluate and eliminate any adverse consequences of new procedures, he says.
Other commentators note that the rights of participants and progeny in assisted reproduction are still undefined. Laws vary widely from state to state on whether a child conceived by donor insemination has the right to know the identity of her biological father. We never resolved the issues surrounding artificial insemination, says George Annas, a professor of law, medicine, and public health at Boston University. We just act like we did. And then we import these issues into the new technology.
With the rapid advances in assisted-reproduction techniques, the ethical and legal issues can only become more complicated, and the task of resolving them will fall to future generations. But that may be fitting, if it’s the children of assisted reproduction who pass judgment on the technology that helped create them.