This story was originally published in our Sept/Oct 2023 issue as "Effective Altruism Goes Viral" Click here to subscribe to read more stories like this one.
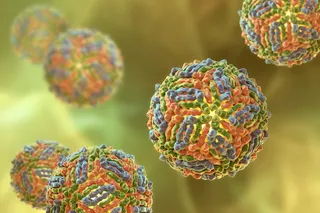
Paresh Patel used to be afraid of needles. Then he volunteered to catch COVID-19. When an email arrived with news that scientists at the University of Oxford in the U.K. were looking for volunteers willing to be infected with the SARS-CoV-2 virus, Patel signed up. He had already caught and survived COVID in October 2020. Other than losing his senses of smell and taste for a few days, the experience was unremarkable.
And at 27 years old, he was young, fit, and had no preexisting conditions, so he wasn’t worried about possible risks like blood clots, breathing difficulties, or even death.
“The only thing, weirdly, that I was worried about was the needles,” he says. Patel hoped that he could help scientists study the ...