The medical record is surprisingly rich with bumbles and quirks, bold moves and devil-may-care experimentation. But important and interesting discoveries have come from these often outrageous acts: by sheer accident, through daring self-sacrifice, from people eccentric enough to look at medical issues through an equally unconventional perspective.
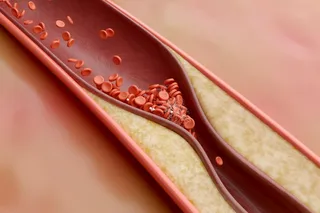
Here’s a look at 10 successes from the annals of the avant-garde that actually worked, along with a brief analysis of their continuing impact on areas as diverse as heart disease, pain management, gastroenterology and seat belts.
This Is Spinal Tap: The Bizarre Origins of Epidurals
German surgeon August Bier remains best known for two things: First, the quote “A professor is a gentleman with a different point of view.” Second, the way he embodied that different point of view while pioneering spinal anesthesia as a surgical procedure.
Inspired by the work of New York neurologist James Corning, who experimented with injections of ...